Inhaled Corticosteroids Downregulates The SARS-CoV-2 Receptor ACE2 In COPD Through Suppression Of Type I Interferon
Source: Inhaled Corticosteroids And COVID-19 Jun 15, 2020 4 years, 10 months, 1 week, 2 days, 16 hours, 2 minutes ago
Inhaled corticosteroids could be the reason that many COPD patients do not seem to be affected by the COVID-19 disease despite the earlier assumptions that most COPD patients were more likely to get sickened badly by the SARS-CoV-2 coronavirus. However the few that do contract the COVID-19, normally end up in extremely severe conditions.
A new study by researchers from Imperial College London that also involved teams from London BioScience Innovation Centre, University of Newcastle and also Royal Brompton & Harefield NHS Trust has found that inhaled corticosteroids reduces the expression of ACE-2 receptors in the endothelial linings of the respiratory tract.
https://www.biorxiv.org/content/10.1101/2020.06.13.149039v1.full.pdf+html
The research finds are yet to have been peer-reviewed and were published on a preprint server.
The research led by Dr Aran Singanayagam PhD. MRCP from the National Heart and Lung Institute at Imperial College, involved both animal models in the first part and a human clinical trial involving a cohort of 40 patients showed that inhaled corticosteroids reduced the expression of ACE-2 receptors in the endothelial cells of the respiratory tract, hence reducing the capability of the SARS-CoV-2 coronavirus to find targets for binding.
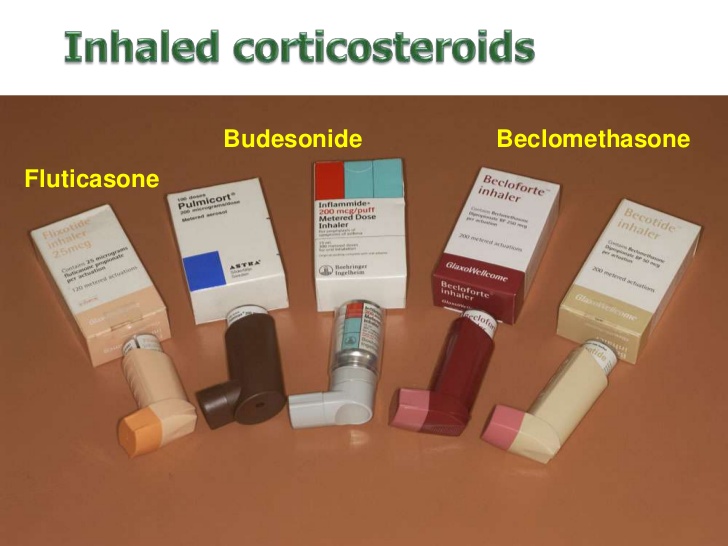
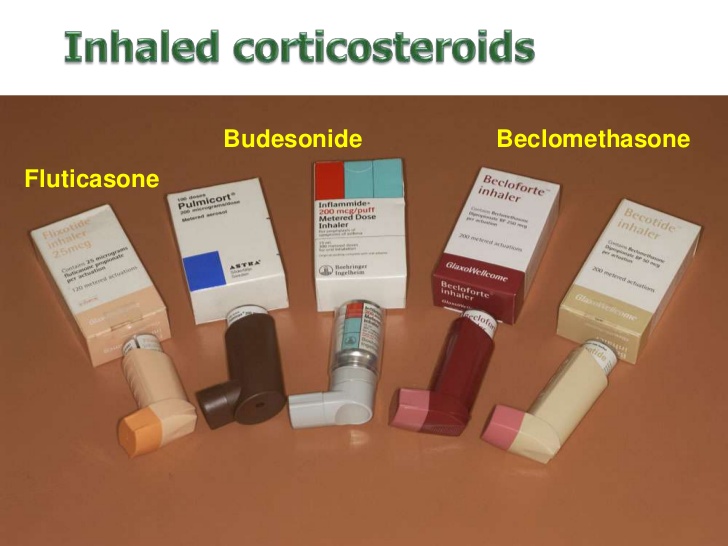
Initial reports of hospitalized COVID-19 cases have shown relatively low frequency of chronic lung diseases such as chronic obstructive pulmonary disease (COPD) but increased risk of adverse outcome. The mechanisms of altered susceptibility to viral acquisition and/or severe disease in at-risk groups are poorly understood. Inhaled corticosteroids (ICS) are widely used in the treatment of COPD but the extent to which these therapies protect or expose patients with a COPD to risk of increased COVID-19 severity is unknown.
The study, using a combination of human and animal in vitro and in vivo disease models, the researchers showed that ICS administration attenuates pulmonary expression of the SARS-CoV2 viral entry receptor angiotensin-converting enzyme (ACE)-2. This effect was mechanistically driven by suppression of type I interferon as exogenous interferon-β reversed ACE2 downregulation by ICS. Mice deficient in the type I interferon-α/β receptor (Ifnar1−/−) also had reduced expression of ACE2. Collectively, these data suggest that use of ICS therapies in COPD reduces expression of the SARS-CoV2 entry receptor ACE2 and this effect may thus contribute to altered susceptibility to COVID-19 in patients with COPD.
However the researchers warned that it is important to note that there is evidence to suggest that downregulation of ACE2 could also theoretically worsen outcome. In mouse models of experimentally-induced acid aspiration and sepsis, genetic deletion of Ace2 worsens acute lung injury, an effect that is partially rescued by recombinant ACE2 administration. ACE2 also degrades angiotensin II which can drive production of proinflammatory cytokines which may be detrimental in the context of the hyper-inflammation that is characteristic in severe COVID-19 .
Downregulation of ACE2 by ICS could therefore remove critical homeostatic protective functions within the lungs and thereby promote severe disease in COVID-19.
ICS use can also impart a number of other detrimental effects on innate immunity to other respiratory viruses (which may also occur in the context of SARS-CoV-2 infection) including suppression of type-I interferon leading to increased virus replication and virus-induced pathology including mucus hypersecretion and secondary bacterial infection.
Hence the researchers therefore cannot currently ascertain whether the clear suppressive effect of ICS upon ACE2 expression shown in the studies would overall have protective or detrimental effects in the context of clinical disease.
Further functional manipulation experiments (e.g. SARS-CoV-2 challenge in ICS treated ACE2 depleted animals) coupled with prospective studies of ICS use as a predictor of susceptibility to SARS-CoV-2 infection are required to understand the direct implications of this effect. If ACE2 downregulation does confer protection against SARS-CoV-2 infection then only will the results suggest that these therapies should be continued stringently in subjects with asthma and COPD. It may also indicate that therapies that are currently in trials, such as recombinant IFN-β, could theoretically induce the adverse effect of increasing ACE2 and promoting greater viral entry.
For more about
inhaled corticosteroids and COVID-19, keep on logging to Thailand Medical News.