Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 12, 2024 5 months, 6 days, 8 hours, 15 minutes ago
Medical News: Exploring the Role of Cytokines in Schizophrenia
Researchers at Patton State Hospital in California-USA have presented a novel theory on schizophrenia, suggesting that interleukin-22 (IL-22) may be key to addressing the complexities of this condition. IL-22, a cytokine produced by specific immune cells, appears to have a role in regulating the body’s barriers, like the gut lining and the blood-brain barrier. The theory proposes that enhancing IL-22 levels might improve symptoms and even reverse some of the damage seen in schizophrenia. This
Medical News report explores the new study in which IL-22’s protective and repair functions are linked to schizophrenia outcomes.
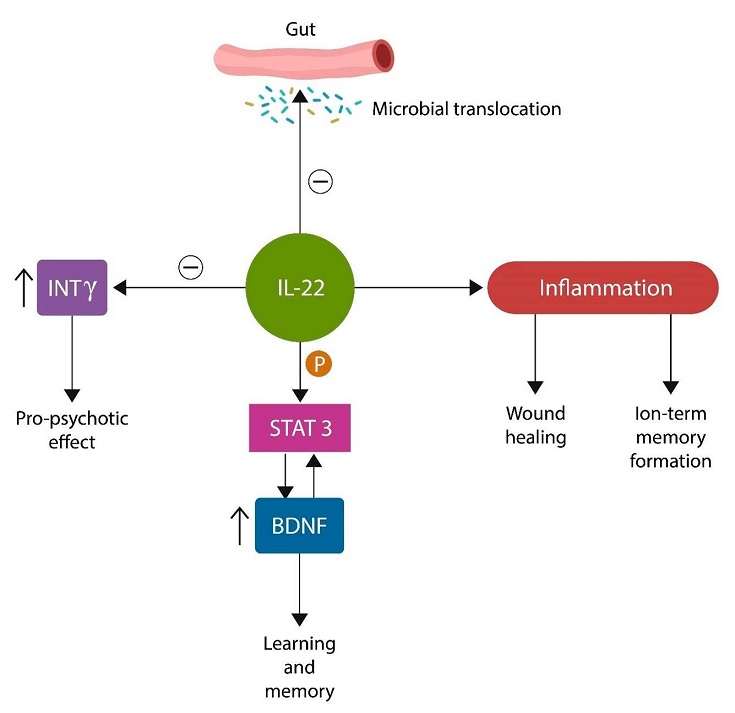
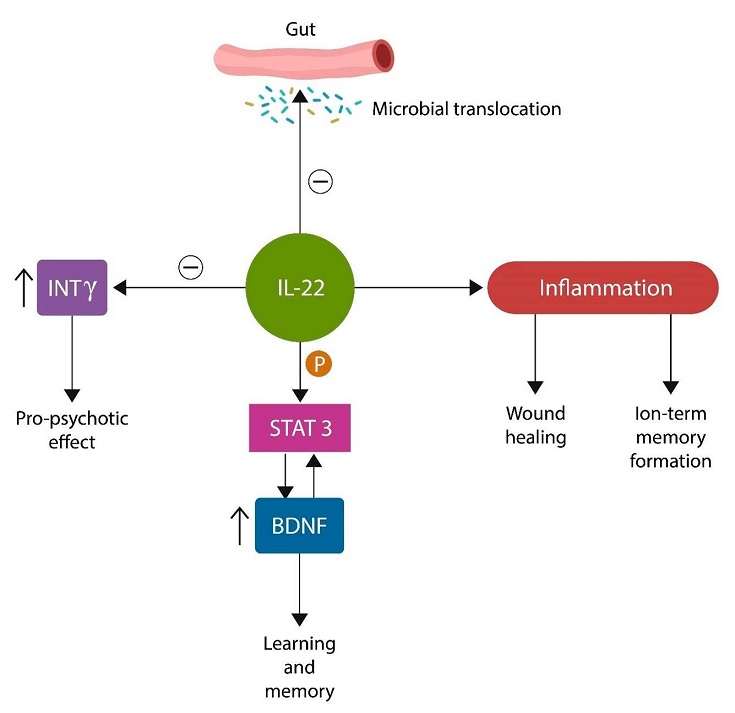 Graphical Abstract - Interleukin-22 Could Offer a New Hope for Schizophrenia Treatment
Graphical Abstract - Interleukin-22 Could Offer a New Hope for Schizophrenia Treatment
Schizophrenia is a serious mental illness characterized by relapses, cognitive decline, and reduced functionality in daily life. Current treatments often fall short of restoring patients’ lives, and relapse remains a common issue. This article will delve into the study findings that reveal how low levels of IL-22, possibly caused by gut and environmental issues, might exacerbate brain inflammation and tissue damage in schizophrenia.
Understanding the Gut-Brain Connection in Mental Health
The research team highlights that while antipsychotic drugs offer symptom relief, they do not prevent the ongoing loss of gray matter in the brain. A possible reason is the impact of inflammation and microbial translocation from the gut to the brain. Researchers propose that gut permeability, resulting from insufficient IL-22, may allow harmful bacteria to move into the bloodstream and eventually reach the brain, worsening schizophrenia symptoms.
IL-22 acts as a “guardian” for the gut lining, helping to maintain its integrity. By regulating gut permeability, it prevents bacteria and toxins from entering the bloodstream. When IL-22 levels are low, this barrier weakens, leading to bacterial migration that triggers inflammation, potentially affecting the brain. Researchers argue that this inflammatory process may contribute to the progressive brain damage observed in schizophrenia.
Key Findings: The Potential of IL-22 in Schizophrenia Management
This theory is based on the understanding that IL-22 interacts with brain-derived neurotrophic factor (BDNF), which is crucial for brain health, memory, and cognitive function. When IL-22 is diminished, BDNF levels drop, leading to a higher risk of brain atrophy and cognitive impairment. By increasing IL-22, it may be possible to preserve BDNF levels, thereby protecting the brain from cognitive decline and damage.
The study reveals that supplementing IL-22 could strengthen the gut and blood-brain barriers, reduce inflammation, and help restore brain tissue. This approach could address the underlying causes of schizophrenia instead of merely alleviating symptoms.
In their report, the researchers propose a future treatment involving recombinant IL-22, a synthetic form that could be administered to p
atients. Initial studies have shown promising results, with IL-22 improving gut barrier function and reducing inflammation in conditions like inflammatory bowel disease and HIV. The authors believe that similar benefits could be achieved for individuals with schizophrenia.
Potential Treatments and Future Research
The study proposes various treatment options beyond traditional antipsychotic medications. These include therapies targeting mitochondrial health, lipid membrane integrity, and the aryl hydrocarbon receptor (AhR), which influences IL-22 levels. Mitochondrial transfer therapy, a treatment involving the transfer of healthy mitochondria to brain cells, has shown promise in animal studies, while membrane lipid replacement therapy may improve cell membrane function and protect against oxidative damage.
The researchers also note the potential of AhR antagonists to reduce inflammation. When activated, AhR can disrupt normal gut barrier function, allowing toxins to pass into the bloodstream. Certain natural and synthetic AhR antagonists, such as quercetin and synthetic compounds like CH-223191, might help counteract this effect, supporting the brain’s health by preventing inflammatory agents from reaching it.
Conclusions and the Path Ahead
This emerging approach offers new hope for improving the lives of individuals with schizophrenia. By addressing the root causes of inflammation and brain damage, IL-22-based treatments could potentially slow or even reverse the progression of the disease. While much more research is needed to confirm the efficacy and safety of these therapies, the study suggests that focusing on cytokines like IL-22 may be a promising avenue.
The study findings were published in the peer-reviewed International Journal of Molecular Sciences.
https://www.mdpi.com/1422-0067/25/22/12110
For the latest on Schizophrenia, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/schizophrenia-and-the-role-of-adenosine
https://www.thailandmedical.news/news/the-whole-body-perspective-and-the-role-of-mirna-143-in-schizophrenia
https://www.thailandmedical.news/news/japanese-case-study-shows-new-onset-of-schizophrenia-in-adolescent-post-covid-19
https://www.thailandmedical.news/news/study-finds-that-cannabis-use-disorder-in-young-males-leads-to-higher-risk-of-developing-schizophrenia
https://www.thailandmedical.news/news/schizophrenia-could-be-due-to-niacin(vitamin-b3)-deficiency-and--body%E2%80%99s-inability-to-use-it-due-to-gene-variant-naprt1