Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 29, 2024 1 year, 2 months, 1 week, 6 days, 21 hours, 37 minutes ago
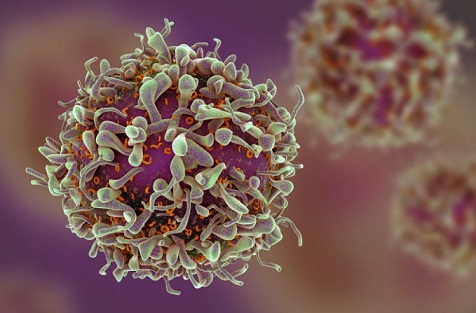
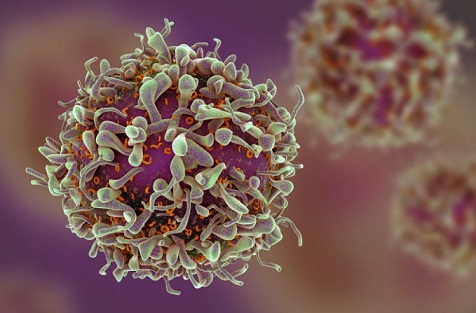
Medical News: Researchers from several Italian institutions have identified a unique group of immune cells, T
R3-56 cells, that could be a key factor in understanding why some patients develop severe COVID-19, while others do not. The study, conducted by teams from the University of Basilicata, the University of Naples "Federico II", and CEINGE-Biotecnologie Avanzate, sheds new light on the immune response to SARS-CoV-2, the virus responsible for the COVID-19 pandemic. This
Medical News report explores the details of their findings and explains what it means for future treatments.
 Italian study discovers new subtype of T-cells as immune players in COVID-19
Immune Responses in COVID-19: A Complex Landscape
Italian study discovers new subtype of T-cells as immune players in COVID-19
Immune Responses in COVID-19: A Complex Landscape
Since the emergence of COVID-19, caused by SARS-CoV-2, scientists have been working tirelessly to understand the immune response to the virus. While many infected individuals experience mild or moderate symptoms, others progress to severe conditions, requiring hospitalization, oxygen support, or even mechanical ventilation. Severe COVID-19 is often associated with an overreaction of the immune system, known as a "cytokine storm," which can result in tissue damage and multi-organ failure.
This study focused on identifying differences in immune responses among COVID-19 patients, specifically looking at the role of a unique immune cell population: the T
R3-56 cells. These cells are part of the CD3+CD56+ T cell family, which has been recognized for its involvement in various immune processes. However, the specific role of T
R3-56 cells in viral infections, particularly in COVID-19, had not been thoroughly investigated before this research.
What Are TR3-56 Cells?
T
R3-56 cells are a subtype of immune cells that exhibit characteristics of both T cells and natural killer (NK) cells, giving them a dual role in the immune system. Previous studies had shown that these cells are involved in regulating immune responses in autoimmune diseases and certain types of cancer. However, their function in viral infections, such as COVID-19, remained unclear until this study.
The research teams analyzed blood samples from hospitalized COVID-19 patients during the first two waves of the pandemic in 2020 and 2021. They grouped the patients based on the severity of their condition, as classified by the World Health Organization (WHO). The study included patients who had not received any treatment before hospitalization to avoid confounding factors.
The researchers found that patients with more severe COVID-19 had higher levels of T
R3-56 cells compared to those with milder forms of the disease. Interestingly, the presence of these cells was particularly elevated in patients requiring high levels of oxygen support or mechanical ventilation.
TR3-56 Cells: A Marker for Severe COVID-19?
This article reveals that the re
search team believes T
R3-56 cells may serve as a biomarker for severe COVID-19. In other words, higher levels of these cells could indicate a more serious form of the disease. The researchers suggest that measuring T
R3-56 cell levels in COVID-19 patients could help doctors identify those at risk of developing severe complications, allowing for more targeted treatment strategies.
One of the key findings of the study was that the number of T
R3-56 cells was positively correlated with other immune cells involved in the body's defense against the virus. Specifically, the researchers found that T
R3-56 cells were linked to higher levels of cytotoxic T cells (CTLs) and natural killer (NK) cells, both of which play crucial roles in attacking virus-infected cells. This suggests that T
R3-56 cells may enhance the immune response by supporting the activity of these other cell types.
The Role of TR3-56 Cells in Immune Regulation
In addition to their potential as a marker for severe COVID-19, T
R3-56 cells appear to have a regulatory function in the immune system. In patients with severe COVID-19, the immune system often becomes overactive, leading to the release of excessive inflammatory molecules, including cytokines such as tumor necrosis factor-alpha (TNF-α). This "cytokine storm" can cause significant tissue damage, contributing to the worsening of symptoms.
The researchers found that T
R3-56 cells were more abundant in patients with higher levels of TNF-α, suggesting that these cells might play a role in modulating the inflammatory response. By regulating the activity of other immune cells, T
R3-56 cells could help prevent the immune system from going into overdrive, thereby reducing the risk of severe inflammation and tissue damage.
Interestingly, the study also revealed that T
R3-56 cells were associated with higher levels of interleukin-17 (IL-17), a cytokine involved in recruiting immune cells to infection sites. This connection between T
R3-56 cells and IL-17 further supports the idea that T
R3-56 cells are actively involved in managing the immune response during COVID-19.
Implications for Treatment
The identification of T
R3-56 cells as a key player in the immune response to COVID-19 opens up new possibilities for treating the disease. Targeting these cells could provide a way to enhance the body's natural defense mechanisms against the virus, while also preventing the immune system from becoming overactive.
One potential approach could involve boosting the activity of T
R3-56 cells in patients with mild or moderate COVID-19, helping their immune system eliminate the virus before it progresses to a more severe stage. Conversely, in patients with severe COVID-19, therapies could be developed to harness the regulatory functions of T
R3-56 cells, reducing inflammation and preventing complications such as acute respiratory distress syndrome (ARDS).
Study Limitations and Future Research
While the findings of this study are promising, there are some limitations to consider. The study was conducted on patients from the first two waves of the pandemic, and the SARS-CoV-2 virus has undergone several mutations since then. It remains unclear whether the findings would apply to newer variants of the virus, such as Omicron.
Additionally, the study did not include a control group of healthy individuals or patients with other viral infections. Future research will need to investigate whether T
R3-56 cells play a similar role in other diseases or if their involvement is unique to COVID-19.
Conclusion: A New Frontier in COVID-19 Research
In summary, the discovery of T
R3-56 cells as a key component of the immune response to COVID-19 offers exciting new possibilities for understanding and treating the disease. These cells appear to play a dual role in both enhancing the immune response and regulating inflammation, making them an important target for future therapies.
As researchers continue to explore the potential of T
R3-56 cells, their findings could lead to new diagnostic tools and treatments that help protect vulnerable patients from the worst effects of COVID-19.
The study findings were published in the peer-reviewed International Journal of Molecular Sciences.
https://www.mdpi.com/1422-0067/25/19/10465
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/omicron-variants-with-g252v-mutation-show-greater-impact-on-t-cells-and-b-cells
https://www.thailandmedical.news/news/uk-study-shows-sars-cov-2-causes-prolonged-change-to-airway-immune-landscape-with-evidence-of-cell-death-due-to-ongoing-activation-of-cytotoxic-t-cell