Japanese Scientists Identify New Fibrinolytic Biomarkers That Can Predict Those At Risk For COVID-19 Severity
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 09, 2024 1 year, 1 month, 5 days, 21 hours ago
COVID-19 News: The global repercussions of the COVID-19 pandemic have been profound, causing unprecedented challenges to healthcare systems worldwide. The surge in infections has strained hospitals, disrupting routine medical services and complicating the management of patients with symptoms ranging from mild to severe, necessitating medical intervention. Recognizing the urgency to identify high-risk patients for more targeted care, researchers have delved into identifying biomarkers that can predict the severity of the disease.
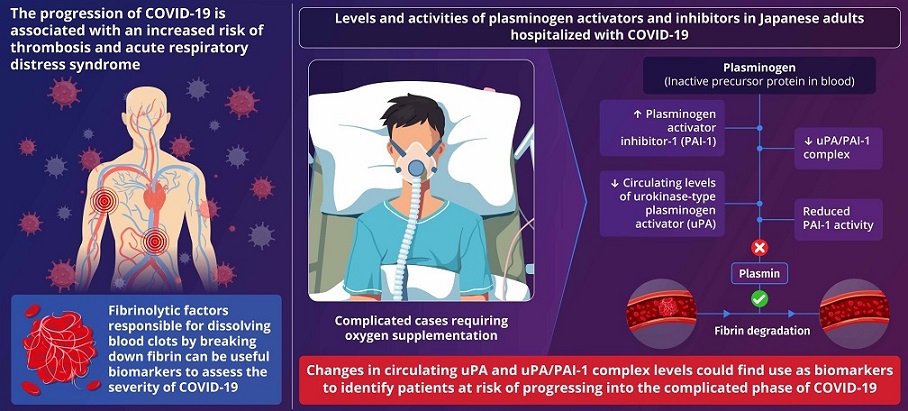
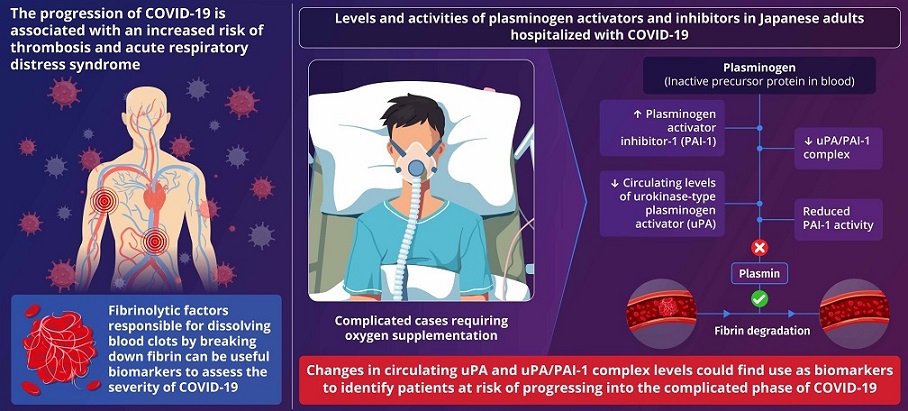 Graphical Abstract - New Fibrinolytic Biomarkers That Can Predict Those At Risk For COVID-19 Severity
Graphical Abstract - New Fibrinolytic Biomarkers That Can Predict Those At Risk For COVID-19 Severity
A recent groundbreaking study conducted by researchers from Juntendo University in Japan that is covered in this
COVID-19 News report, led by specially appointed Senior Associate Professor Dr Koichi Hattori, Associate Professor Dr Beate Heissig, and Japan Society for the Promotion of Science researcher Dr Tetiana Yatsenko, has shed light on novel fibrinolytic biomarkers. These biomarkers may serve as indicators to identify individuals at risk of progressing to a severe stage of COVID-19.
Plasminogen as a Key Player
One specific protein that captured the researchers' attention is plasminogen. When activated to plasmin, it plays a crucial role in dissolving blood clots by breaking down fibrin, the mesh-like structure that holds the clot together. Intriguingly, individuals with COVID-19 often exhibit lower levels of this critical protein. Dr Hattori emphasizes, "Identifying high-risk patients, such as those who might require oxygen supplementation as early as possible, will save lives."
Examining Fibrinolytic Protein
The research focused on three proteins associated with blood clot formation: urokinase-type plasminogen activator (uPA), tissue-type plasminogen activator (tPA), and plasminogen activator inhibitor-1 (PAI-1). These proteins play a pivotal role in regulating plasminogen-plasmin levels.
PAI-1: A Key Indicator of Severity
Patients requiring oxygen supplementation displayed elevated levels of PAI-1, a protein inhibiting plasminogen activators by forming complexes. Interestingly, the levels of active PAI-1 that restrict plasmin activation remained consistent across all groups, suggesting its potential as a biomarker for disease severity.
Distinctive Patterns of uPA
In contrast, uPA levels were lower in COVID-19 patients compared to the healthy control group, with the lowest levels observed in patients requiring oxygen supplementation. The study highlighted that significant decreases in circulating uPA and uPA/PAI-1 complex levels could serve as novel biomarkers indicating the severity of COVID-19.
Correlations with Acute Respiratory Distress Syndrome (ARDS)
The researchers identified robust correlations between fibrinolytic proteins and complications such as ARDS and lymphopenia, commonly observed
in severe cases of COVID-19. PAI-1 levels were positively correlated with severe ARDS, while uPA/PAI-1 complex levels exhibited a negative correlation with ARDS, emphasizing their potential as prognostic indicators.
Endothelial Dysfunction and Inflammation
Elevated PAI-1 levels were found to correlate with soluble urokinase plasminogen activator receptor (suPAR) and soluble vascular cell adhesion molecule-1 (sVCAM-1). These proteins are released by endothelial cells in response to inflammation triggered by the SARS-CoV-2 virus, suggesting that heightened PAI-1 levels could indicate endothelial dysfunction associated with COVID-19.
Implications for Patient Care
Dr Hattori emphasized the significance of these findings, stating, "By identifying individuals who are at risk of progressing to a severe stage of COVID-19, we can reduce the strain on medical facilities as we can reserve emergency beds for those who might experience worsening of the disease and provide medical care tailored to the specific condition of each patient."
The Complexity of Fibrinolytic Factors
Delving further into the study, the researchers explored various aspects of the fibrinolytic system. The two-chain urokinase-type plasminogen activator (uPA), with its high profibrinolytic activity, is known for its role in cell-associated plasmin generation. In its free form, uPA is promptly inhibited by active PAI-1. The study emphasized the importance of analyzing fibrinolytic factors in both free and complexed forms to understand their biological functions fully.
Ethnic Differences and Thrombosis Incidence
The research also addressed ethnic differences, comparing the fibrinolytic status of healthy Japanese and European subjects. A trend towards higher active PAI-1 levels was found in Europeans compared to Japanese subjects. This aligns with epidemiological studies showing lower thrombosis incidence in Asian populations compared to other ethnic groups. Genetic polymorphisms and lifestyle factors may contribute to these variations, with potential implications for the severity of COVID-19 outcomes.
Understanding Disease Stage-Dependent Changes
The study meticulously examined the phenotypic and clinical presentation of COVID-19 patients, categorizing them into uncomplicated and complicated phases. Despite elevated coagulation markers in the complicated phase, patients in this group had nearly average active PAI-1 values. This unique fibrinolytic status, combined with high tPA/PAI-1 and plasmin/α2AP complexes, suggested a lower risk of thrombosis in the Japanese cohort.
Association with Comorbidities
Considering the influence of comorbidities on fibrinolytic response, the researchers explored subgroups with conditions like diabetes, hypertension, and heart disease. The study found associations between high uncomplexed PAI-1 levels and diabetes, while low uPA/PAI-1 complex levels were linked to hypertension and heart disease. These findings highlight the multifaceted nature of fibrinolytic factors in the context of COVID-19 severity and associated comorbidities.
Correlation with Inflammatory Response
The study further delved into the intricate relationship between fibrinolytic factors and the inflammatory response. Increases in inflammatory cytokines such as CRP, IL6, and IL1β were linked with high total PAI-1 antigen and low uPA/PAI-1 complex levels. These correlations underscore the role of PAI-1 in reflecting the inflammatory response associated with COVID-19.
Implications for Future Research
As the research unravels the complex interplay of fibrinolytic factors in COVID-19, the authors emphasize the need for further studies to understand the functional consequences of uPA, uPA/PAI-1 complexes, and tPA/PAI-1 complexes in inflammation. The data suggest that analyzing uPA, uPA/PAI-1 complex, and non-complexed PAI-1 should be integrated into larger clinical trials to validate their utility as prognostic markers. Moreover, longitudinal studies tracking fibrinolytic biomarker dynamics throughout the course of COVID-19 could provide insights into disease progression and inform therapeutic interventions.
Expanding the scope of research to encompass diverse populations is crucial for understanding the ethnic variations observed in fibrinolytic profiles. Investigating genetic polymorphisms and their impact on fibrinolytic responses could elucidate disparities in COVID-19 outcomes among different ethnic groups. Furthermore, exploring the influence of lifestyle factors, such as diet and physical activity, on fibrinolytic function may uncover modifiable risk factors for severe COVID-19.
In parallel, efforts to develop point-of-care diagnostic tools based on fibrinolytic biomarkers hold promise for enhancing patient care and resource allocation.
Potential for Portable Test Kits
The study's implications extend beyond understanding disease severity, as it paves the way for the development of portable test kits. Such kits could enhance screening processes, enabling more targeted healthcare interventions. Dr Hattori and his team have taken a significant step by applying for a patent based on these groundbreaking findings.
Portable test kits capable of rapidly quantifying plasminogen, uPA, and PAI-1 levels could facilitate early risk stratification and guide treatment decisions in clinical settings with limited resources. Integration of these biomarkers into existing diagnostic algorithms may improve the accuracy of prognostic assessments and optimize patient outcomes.
Conclusions
Collaborative endeavors between researchers, clinicians, and industry partners are essential for translating scientific discoveries into actionable strategies for combating COVID-19. Multidisciplinary approaches combining expertise in molecular biology, immunology, and clinical medicine will drive innovation and accelerate the development of effective diagnostic and therapeutic solutions. Furthermore, fostering international collaborations and data sharing initiatives can expedite the identification of biomarkers with global relevance and facilitate the implementation of standardized diagnostic protocols.
Beyond COVID-19, the insights gained from studying fibrinolytic biomarkers may have broader implications for understanding thrombotic disorders and inflammatory diseases. Chronic conditions such as cardiovascular disease, diabetes, and cancer are characterized by dysregulated fibrinolysis and heightened inflammation, highlighting the potential utility of fibrinolytic markers as prognostic indicators and therapeutic targets. By elucidating the underlying mechanisms linking fibrinolysis to disease pathogenesis, researchers can advance precision medicine approaches tailored to individual patient profiles.
In conclusion, the study conducted by researchers from Juntendo University represents a significant advancement in our understanding of fibrinolytic biomarkers in COVID-19. By elucidating the complex interplay between fibrinolytic proteins and disease severity, the findings offer valuable insights into the pathophysiology of COVID-19 and underscore the importance of personalized medicine approaches. Moving forward, continued research efforts aimed at validating and refining fibrinolytic biomarkers will be instrumental in improving risk stratification, guiding clinical management, and ultimately saving lives in the ongoing battle against COVID-19 and beyond.
The study findings were published in the peer reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1299792/full
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-diagnostics-researchers-uncover-new-protein-biomarker-supar-to-identify-covid-19-patients-at-risk-of-acute-kidney-injury-aki
https://www.thailandmedical.news/news/latest-covid-19-news-protein-supar-identified-as-new-biomarker-for-acute-respiratory-failure-in-covid-19-patients