Johns Hopkins Study Discovers That COVID-19 Alters Human Respiratory Cells in Surprising Ways
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 02, 2024 4 months, 1 week, 4 days, 8 hours, 43 minutes ago
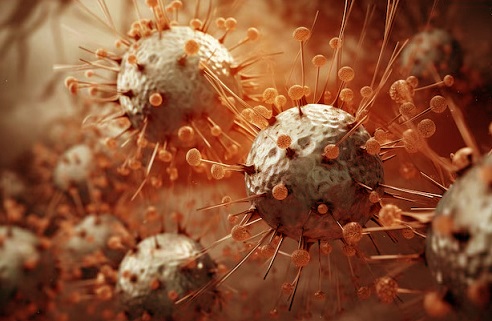
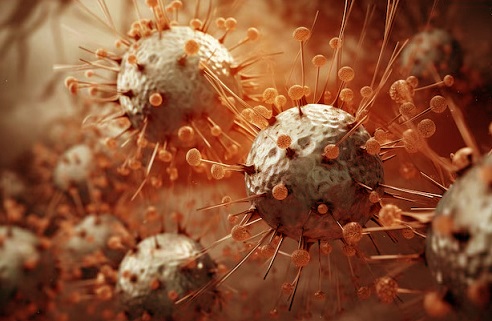
Medical News: Scientists from the Johns Hopkins Bloomberg School of Public Health and the Johns Hopkins School of Medicine-USA have revealed surprising details about how the COVID-19 virus affects human respiratory cells. This research uncovers how SARS-CoV-2, the virus causing COVID-19, impacts energy production in cells and changes their structure. These insights could help explain why the virus has led to such severe outcomes and prolonged health issues compared to the influenza virus.
 Johns Hopkins Study Discovers That COVID-19 Alters Human Respiratory Cells in Surprising Ways
Johns Hopkins Study Discovers That COVID-19 Alters Human Respiratory Cells in Surprising Ways
The study focuses on the effects of the virus on human nasal epithelial cells, the body’s frontline defense against respiratory viruses. By comparing the responses of these cells when infected with either SARS-CoV-2 or the influenza virus, researchers identified unique patterns. This
Medical News report highlights how these findings provide a clearer picture of why COVID-19 behaves differently from the flu.
How the Virus Affects Cell Function and cell Structure
Using advanced techniques like RNA sequencing, the research team observed how SARS-CoV-2 disrupts mitochondrial function in respiratory cells. Mitochondria are essential for producing the energy cells need to perform various tasks. When the virus infects these cells, it reduces the activity of key mitochondrial proteins such as SIRT3 and TOMM22. This weakens the cells' energy production, shifting them to a less efficient energy pathway known as glycolysis.
Additionally, SARS-CoV-2 causes notable structural changes. The spike protein, which facilitates the virus's entry into cells, triggers a rearrangement of the cell’s cytoskeleton. This protein reduces levels of cofilin-1, a critical molecule that regulates cell structure. The result is a buildup of polymerized actin, causing changes that might impair the cells' ability to function and recover from injury.
Why These Changes Matter
The combined effects of mitochondrial dysfunction and cytoskeletal changes may help cells survive the initial infection but come at a cost. These adaptations could lead to the chronic symptoms many COVID-19 patients experience, such as fatigue and long-term lung issues. By contrast, the influenza virus, while also damaging, does not cause the same level of disruption to mitochondrial function or cell structure.
A Window into Long-Term Impacts
One of the most striking observations from this study is how SARS-CoV-2 modifies cell behavior to favor survival during infection. However, these changes alter the fundamental properties of the cells. For example, the decrease in mitochondrial activity was accompanied by increased extracellular acidification, suggesting a shift in how energy is generated. This could explain why some patients face prolonged recovery times and lingering symptoms, often referred to as long COVID.
Further experiments with pseudoviruses that mimic SARS-CoV-2 confirmed the role of its spike protein in these changes. This spike protein alone
was enough to induce the cellular responses observed, highlighting its central role in the virus's impact on human health.
Implications for Treatment
Understanding these cellular mechanisms opens the door for new therapeutic strategies. Targeting mitochondrial pathways or stabilizing cytoskeletal functions could be potential approaches to mitigate the virus's long-term effects.
The Bigger Picture
COVID-19 has changed the world, not just in terms of public health but also in how it has expanded our understanding of viral diseases. Studies like this emphasize the importance of exploring the cellular-level impacts of infections. Such insights not only explain the immediate effects of diseases but also provide critical clues about their long-term consequences.
Conclusion
The research highlights how SARS-CoV-2 uniquely impacts human respiratory cells by altering their energy production and structure. These changes, while initially beneficial for cell survival, could pave the way for chronic health issues. This duality of survival and dysfunction helps explain why COVID-19 often leads to more severe and long-lasting outcomes compared to influenza.
The study findings were published in the peer-reviewed journal: mBio.
https://www.sciencedirect.com/org/science/article/pii/S2150751123004380
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-linked-to-dangerous-lung-scarring-through-mast-cell-activation
https://www.thailandmedical.news/news/chinese-study-uncovers-impact-of-covid-19-on-cancer-progression
https://www.thailandmedical.news/news/polish-study-finds-that-covid-19-stiffens-blood-vessel-cells-and-disrupts-their-structure