Key findings from the latest research on bystander monocytic cells and their role in COVID-19 inflammation
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 08, 2024 7 months, 2 weeks, 4 days, 12 hours, 25 minutes ago
Medical News: Understanding the Role of Immune Cells in COVID-19
As COVID-19 continues to be a global health concern, researchers have sought to better understand how the immune system reacts to the SARS-CoV-2 virus, particularly the role of monocytes and macrophages. A recent study from a team of researchers from Johns Hopkins University School of Medicine-USA, Johns Hopkins Bloomberg School of Public Health-USA, and Oregon Health and Science University-USA delves into the intricacies of how bystander monocytic cells drive an infection-independent NLRP3 inflammasome response to the virus. This
Medical News report highlights key findings from this research, offering insights into potential therapeutic strategies. The study focuses on inflammation, a major hallmark of severe COVID-19, and how certain immune cells respond to the virus, even without direct infection.
 Key findings from the latest research on bystander monocytic cells and their role in
Key findings from the latest research on bystander monocytic cells and their role in
COVID-19 inflammation
Inflammasomes: The Body's Response to COVID-19
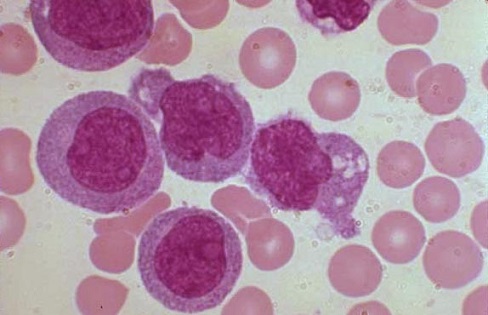
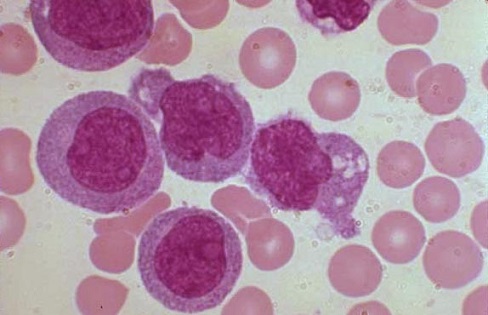
COVID-19 is known for triggering a hyperinflammatory response in many patients, particularly those with severe illness. Monocytes and macrophages are among the immune cells most involved in this response. These cells, when activated, can contribute to severe inflammation. One crucial mechanism that governs this inflammatory reaction is the activation of the NLRP3 inflammasome.
An inflammasome is a multi-protein complex within immune cells, such as monocytes and macrophages, that helps trigger inflammation. It responds to signals like infection or cellular stress. In the case of COVID-19, the activation of the NLRP3 inflammasome has been observed in many patients. However, the mechanisms behind this activation were not well understood until this study explored the infection-independent pathways involved.
Bystander Monocytic Cells: Key Players in Inflammation
The study found that bystander monocytic cells, which are not directly infected by SARS-CoV-2, still play a significant role in the inflammatory response. These cells, through pathways unrelated to direct viral replication, can trigger the NLRP3 inflammasome. The study explains how the presence of the virus in the airways leads to inflammasome activation in macrophages and monocytes without them being directly infected.
The research team used various cell types, including macrophage-like THP-1 cells and human nasal epithelial cell (hNEC) cultures, to understand how SARS-CoV-2 affects the immune system. Interestingly, while SARS-CoV-2 could replicate in nasal epithelial cells, it did not trigger the production of key inflammatory cytokines, such as IL-18 and IL-1β. These cytokines are critical components of the inflammasome activation process. This suggests that macrophages, rather than epithelial cells, are the primary drivers of the inflammasome response.
SARS-CoV-2 and Inflammasome Activation: A Closer Look
One of the most striking findings was that SARS-CoV-2 could induce inflammasome activation in macrophages without relying on viral replication. The
study demonstrated that viral entry into macrophages does not necessarily lead to productive replication, yet the inflammasome is activated. The researchers confirmed that this inflammasome activation was dependent on the NLRP3, ASC, and caspase-1 pathways, which are critical components of the immune response.
Moreover, the study showed that inhibiting key components like IL-1β and IL-18 could help reduce inflammation without increasing viral replication. This is significant because controlling inflammation is a major therapeutic goal in severe COVID-19 cases, where excessive immune responses can lead to organ damage and other complications.
Therapeutic Implications: Targeting Inflammation
Given the findings, therapeutic strategies targeting the NLRP3 inflammasome could offer a promising approach to managing severe COVID-19. The study provides evidence that macrophage-mediated inflammation could be controlled by inhibiting certain inflammatory cytokines like IL-1β and IL-18. This approach has the potential to reduce the harmful effects of the hyperinflammatory response without compromising the body's ability to fight off the virus.
The results from this study suggest that therapies targeting inflammasome activation may help alleviate severe inflammation in COVID-19 patients. This could be particularly valuable in the later stages of the disease, where inflammation tends to cause the most damage. Moreover, the fact that bystander cells (cells not directly infected by the virus) can still drive this inflammatory response highlights the complexity of the immune response in COVID-19.
Expanding Our Understanding of COVID-19
This research advances our understanding of how SARS-CoV-2 interacts with the immune system. One of the study’s important revelations is that the virus does not need to infect monocytes and macrophages directly to trigger an immune response. Instead, bystander cells sense the virus and activate inflammatory pathways. This has broad implications for how we think about viral infections and the immune response.
Additionally, the researchers discovered that the pro-inflammatory cytokines IL-1β and IL-18, while elevated in severe COVID-19, do not inhibit viral replication. This underscores the idea that inflammation, rather than direct viral replication, may be the primary driver of severe disease in COVID-19 patients. By targeting these cytokines, future therapies may be able to reduce inflammation without interfering with the body’s ability to control the virus.
Conclusion: The Path Forward
In conclusion, the study offers critical insights into how SARS-CoV-2 activates inflammation in the body, particularly through bystander monocytic cells. The findings highlight the central role of macrophages in driving the immune response and provide a potential pathway for therapeutic intervention by targeting key inflammatory cytokines like IL-1β and IL-18. These discoveries could pave the way for new treatments that reduce the risk of severe inflammation in COVID-19 patients, ultimately improving outcomes for those most at risk.
For healthcare providers and researchers, this study emphasizes the importance of focusing on the inflammatory response in COVID-19 and not just on viral replication. The potential for targeted therapies that modulate the immune system’s reaction to SARS-CoV-2 could represent a significant breakthrough in the ongoing fight against this global pandemic.
The study findings were published in the peer-reviewed journal: mBio.
https://journals.asm.org/doi/full/10.1128/mbio.00810-24
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-vaccines-causes-persistence-of-spike-protein-in-the-cd16-monocytes-and-makes-sars-cov-2-negative-people-sick-with-pasc-like-sickness
https://www.thailandmedical.news/news/convalescent-covid-19-patients-found-to-have-reduced-monocyte-proportions-and-monocytes-that-were-hyporesponsive-evidence-of-immune-dysregulation