Latest! Stanford Study Finds That Excessive Ventilation Favors SARS-CoV-2 Survival And Spread As Low Humidity Is Conducive For Viruses!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 20, 2024 1 year, 9 months, 1 week, 1 day, 2 hours, 3 minutes ago
COVID-19 News: In the midst of the global COVID-19 pandemic, understanding the intricate dynamics of how respiratory viruses spread in indoor environments has become paramount. Recent groundbreaking research from Stanford University has shed light on a critical factor influencing the survival and transmission of airborne viruses: indoor humidity levels and ventilation practices. This
COVID-19 News report delves deep into the findings of the Stanford study and explores the broader implications for public health strategies aimed at combating airborne viral infections.
 Excessive Ventilation Favors SARS-CoV-2 Survival And Spread
Excessive Ventilation Favors SARS-CoV-2 Survival And Spread
As Low Humidity Is Conducive For Viruses
The study opens a new insight about how clean air strategies should be properly devised and not the garbage currently being spewed online by so called Zero COVID zealots from the End Coronavirus or WHN groups lead by a group of charlatans formerly or currently from the NECSI…it was also these same idiots who also came up with stupid things like “flatten the curve with 1.5 meters distancing” in the early part of the pandemic etc and are now busy promoting the use of fluvoxamine to prevent disease severity in COVID-19! We have certain Thai monks from Mae Hong Song-Thailand being active players in their initiatives and even orchestrating randomized clinical trials involving fluvoxamine with bias and faked study findings!
Unraveling the Relationship Between Indoor Humidity and Viral Transmission
The study conducted at Stanford University focused on the interplay between indoor relative humidity (RH) levels and the concentration of naturally occurring disinfectant compounds, particularly hydrogen peroxide (H2O2), in airborne microdroplets. These microdroplets play a pivotal role in the transmission of respiratory viruses like SARS-CoV-2, as they can remain suspended in the air and potentially infect individuals who come into contact with them.
The research team, led by senior author Professor Richard Zare, discovered a strong correlation between RH levels and the formation of anti-viral compounds within microdroplets. Specifically, they found that maintaining indoor RH levels between 40% and 60% could naturally promote the production of hydrogen peroxide and other disinfectant agents, which have the potential to render viruses ineffective within exhaled droplets.
Professor Zare commented, "Experts have long recommended indoor relative humidity of 40% to 60%, and now this research points to a significant benefit: humidity in this range naturally creates anti-viral compounds in the air's microdroplets.”
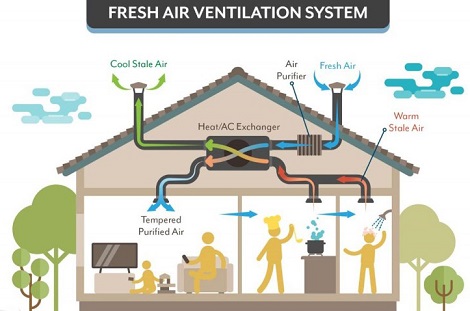
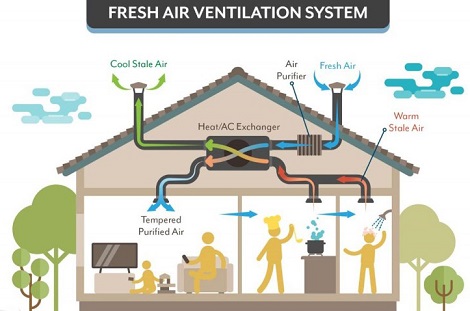
Challenges of Excessive Ventilation
One of the surprising findings of the study was the potential downside of excessive ventilation in indoor spaces. While ventilation is often recommended as a strategy to improve indoor air quality and reduce the risk of viral transmission, the researchers cautioned that excessive ventilation can lead to lower RH levels, which may counteract the bene
fits of air circulation.
Professor Zare emphasized the importance of striking a balance between ventilation and humidity control. Simply increasing air changes per hour, particularly in winter when heating systems are in use, can lead to excessively dry indoor air, creating conditions where viruses can survive longer and remain suspended in the air. This highlights the need for a more nuanced approach to indoor air quality management that considers both ventilation rates and humidity levels.
Seasonality of Respiratory Viruses and Climate Control
The study's findings also provide insights into the seasonality of respiratory illnesses such as COVID-19 and influenza. It's well-known that viral infections tend to be more prevalent during colder months, a trend often attributed to factors like increased indoor gatherings and lower humidity levels due to heating systems.
Natural Floating Disinfectants
Professor Zare's team found that low RH values, typical in winter when heating systems dehydrate indoor air, create conditions where viruses can survive longer and remain airborne. Conversely, higher humidity levels, which are more common in warmer months, promote the formation of disinfectant compounds, potentially reducing the viability of airborne viruses.
Past studies led by Professor Zare revealed that hydrogen peroxide, a common disinfectant, can spontaneously form in water microdroplets. The study team discovered that, as humidity increases, so does the concentration of hydrogen peroxide and other naturally occurring disinfectant agents in the air.
This finding suggests that ventilation aimed at preventing the spread of disease - which tends to dry air out - could be counterproductive and reveals a possible mechanism for the increased number of cases of airborne viruses during the winter months when heating and ventilation are used more often. The study also highlights the possibly beneficial effects of increased humidity for reducing the spread of airborne viruses.
Typically, respiratory illnesses are spread via infected water droplets exhaled when someone coughs, sneezes, or even talks. But water microdroplets might be capable of killing viruses in exhaled droplets, thanks to the abundance of reactive oxygen species, like hydrogen peroxide, on their surfaces.
In order to better comprehend this potential, the researchers studied water microdroplets, around 11 microns in diameter, in a humidity-controlled environment. Using nuclear magnetic resonance and other analysis methods, they measured the concentration of hydrogen peroxide at different temperatures, humidity levels, droplet sizes, and atmospheres.
The findings showed that when they increased the humidity from 15% to 50%, the concentration of hydrogen peroxide increased by a factor of 3.5. From 50% to 95%, the concentration leveled off. So, as humidity increases, so does the concentration of reactive oxygen species and their ability to disinfect.
Professor commented, "When you have low relative humidity, two things happen. One, you do not form these reactive oxygen species as much as you do at higher relative humidity. Number two, the droplet evaporates much more rapidly, and the virus is quite content to be in a dry state and floating around. It becomes very light, and it doesn't fall to the ground for a long time."
The study team is already working on further studies to understand better exactly how reactive species, such as hydrogen peroxide, could reduce the prevalence of viruses in the air. However, the current results suggest that humidity could be an important factor in controlling the spread of airborne viruses. As of now, however, humidity is not considered in disease control plans or recommendations.
Practical Implications for Disease Control Strategies
The implications of this research are significant for public health strategies aimed at controlling airborne viral infections. Traditionally, ventilation has been a primary focus for improving indoor air quality, but the study suggests that a holistic approach that includes humidity control is necessary for optimal results.
Professor Zare recommends implementing humidity control measures alongside ventilation strategies to maintain RH levels within the optimal range of 40% to 60%. This balanced approach can naturally support the formation of disinfectant compounds in airborne microdroplets, contributing to a healthier indoor environment and potentially reducing the spread of respiratory viruses.
Future Research Directions and Technological Innovations
The Stanford study opens new avenues for further research and technological advancements in indoor air quality management. Future studies may explore specific ventilation strategies, such as the use of humidifiers or air conditioning systems with humidity control features, to effectively regulate indoor RH levels while ensuring adequate air circulation.
Collaborations between researchers, virologists, and environmental scientists could lead to the development of innovative technologies that harness humidity as a tool for viral disinfection. For example, humidity-controlled systems that optimize RH levels based on real-time viral transmission data could revolutionize indoor air quality management in healthcare facilities, schools, and other public spaces.
Conclusion: Enhancing Public Health Through Humidity Control
In conclusion, the Stanford study underscores the critical role of indoor humidity levels and ventilation practices in controlling airborne viral infections. By understanding how RH levels influence the formation of disinfectant compounds in airborne microdroplets, researchers and public health experts can refine existing strategies and develop new approaches to mitigate the risk of respiratory illnesses.
As we navigate the ongoing challenges posed by infectious diseases, insights from studies like the one conducted at Stanford University are invaluable for shaping evidence-based interventions and creating healthier indoor environments. By prioritizing optimal indoor humidity levels alongside effective ventilation, we can enhance our defenses against airborne viruses and improve overall public health outcomes. Incorporating humidity control measures into indoor air quality management plans represents a proactive step toward safeguarding individuals and communities against respiratory infections now and in the future.
The study findings were published in the peer reviewed journal: Proceedings of the National Academy of Science.
https://www.pnas.org/doi/10.1073/pnas.2315940121
For the latest
COVID-19 News, keep on logging to Thailand Medical News.