Source: Thailand Medical News Nov 08, 2019 5 years, 5 months, 2 weeks, 4 days, 20 hours, 42 minutes ago
The number of cases of
Legionnaires' disease reached a record high in 2018 not only in the US but globally, more than eight-fold increase since the numbers began to climb nearly two decades ago. Figures from the first 8 months of 2019, shows that it is also increasing and might it another record high.
The US Center for Disease Control and Prevention reported this week 9,933 cases in 2018 of
Legionellosis, which includes both
Legionnaires' disease and Pontiac fever. This do include global figures which are estimated to stand at about 340,000 cases.
Legionnaires' disease made up the vast majority of cases, according to the CDC.
Unfortunately, the problem may be exponentially larger than what's reported to public health officials. The National Academies of Sciences, Engineering, and Medicine estimates that as many as 70,000 people may suffer from the disease each year just in the US alone while globally the figure might be more than 6 times the existing figure, according to a report released in August 2019.
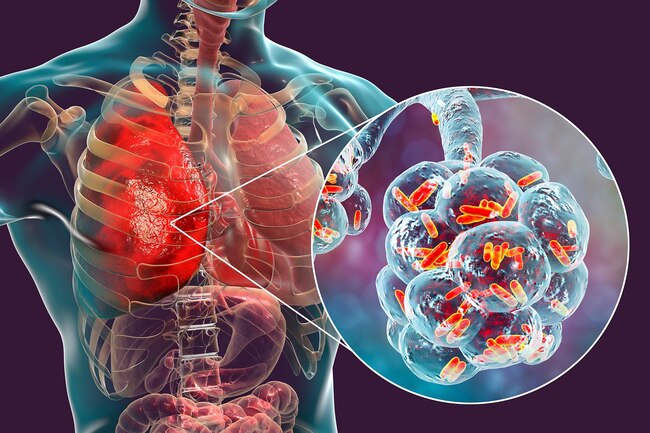
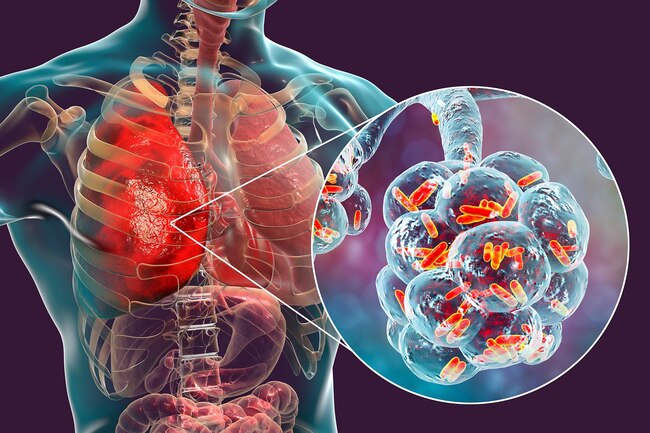
Air cons, hot tubs, hotels and hospitals across the world continue to be hotbeds for the potentially deadly disease, which people contract after inhaling mist or water droplets contaminated with
Legionella bacteria. It causes severe pneumonialike symptoms and kills 10% of those sickened. Nearly one-quarter die if they contract the disease in a health care setting.
Vapour or water that sits stagnant in old pipes, cooling towers or hotel rooms can become a breeding ground for the dangerous bacteria to grow and fester when water is not cool or hot enough. Experts point to a number of causes for the explosion of cases across the country: decaying infrastructure, an aging population, greater testing for the disease, water conservation efforts and even climate change.
Media news has been transfixed by the sometimes deadly cases around the country, from the four fairgoers killed and nearly 150 sickened by a hot tub exhibit at a North Carolina state fair in September to multiple hotel guests struck ill at the Sheraton Atlanta Hotel this summer.
Fighting the problem is an expensive undertaking. The annual costs of treating
Legionnaires' disease, based on hospitalization claims, was US$434 million in 2012, just in the US alone. It has likely grown with the uptick in cases. Flushing out water systems or even redoing them to get rid of the bacteria costs far more. California alone has spent $8.5 million this year cleaning up an outbreak at a Stockton prison that killed one inmate. For facilities, the consequences of finding the bacteria can be catastrophic, even if not deadly. The water often must be shut off, leading to negative media coverage, the potential for lawsuits or financial ruin.
In the city of Washington, D.C., the public psychiatric hospital St. Elizabeths relied on bottled water for weeks this fall after
Legionella bacteria was detected, and some patients filed a suit claiming "inhumane, unsafe, and medically dangerous conditions that risk the health, mental health, and safety" of patients. The suit also alleged, "Patients cannot shower, wash their hands, or use the toilets regularly. Fecal matter, urine, and menstrual blood are accumulating in the bathrooms." The remediation alone has cost more than $1 million, according to The Washington P
ost.
The issue of fear of that kind of financial hit leads building managers to resist testing or actively looking for
Legionella, said Laura Ehlers, who directed the study for the National Academie. And even when facilities have water management plans in place to prevent the bacteria, it still is still showing up.
As cases were reported in Missouri last year, state officials investigated 61 hospitals, nursing homes and hotels from last fall until late this summer, according to a undisclosed document. Seven of those facilities tested positive for
Legionella bacteria even though each had a water management plan in place.
Since 2017, the Centers for Medicare & Medicaid Services has mandated that heath care facilties have such water management plans. But even with a good water management plan,
Legionella risk is ever present, according to Jonathan Garoutte, administrator of the Missouri health department's section for environmental public health. "
Legionella finds places within large complex water systems to hide," he said.
Following a 2015 Bronx, N.Y., outbreak, which killed 16 and sickened 138, the CDC redoubled its efforts, CDC epidemiologist Dr Chris Edens said.
The officials are finding that as temperatures rise and summer extends, that could spur more bacterial growth.
Dr Edens told
Thailand Medical News, "If devices like air conditioning units are used for longer periods of time that could certainly pose a risk."
Dr Edens also pointed to an unusual source: the green building movement. She said LEED-certified buildings and other efforts to conserve water often hold such water at temperatures that are unsafe. "It's made a growth dish for
Legionella," she said.
As more cases have risen, the CDC has increased communication about outbreaks, created a water management toolkit and helped CMS set a 2017 rule requiring health facilities and nursing homes to have a water management plan to reduce the risk of
Legionella.
The Mercy health care system faced two positive Legionella tests in the past year one in its outpatient cancer center in Springfield in May, and another at Mercy Hospital St. Louis in February.
The task of flushing out Mercy's cancer center plumbing after Legionella bacteria was found in four areas required extensive work, according to Mercy spokeswoman Sonya Kullmann. About 75 Mercy employees worked through the weekend to proactively call around 5,200 patients. The hospital system then offered free testing for
Legionnaires' to anyone who did not feel well which 120 people took them up on, costing $30,000. All tested negative.
Worst, the
Legionella bacteria turned out to be a type that does not cause
Legionnaires' disease.
Key question for facilities is how much to proactively guard against the bacteria so they don't end up footing millions of dollars in bills if
Legionella is found. Edens stressed that deciding whether or not to make complex water systems foolproof can be a life or death decision.
"Our message is that cost is worth it," Dr Edens said. "It can prevent people from getting a disease and prevent people from dying."