Long COVID Could Also Be Due To SARS-CoV-2 Dysregulating The Human Host Immune System For Months Including Downregulating Naive T And B Cells!
Source: Long COVID-Immune Dysregulation Jan 15, 2022 3 years, 11 months, 1 week, 5 days, 2 hours, 27 minutes ago
Long COVID: Australian researchers in response to an article that was published by Thailand
Medical News with regards to SARS-CoV-2 coronavirus causing immunodeficiency issues in all those that had been infected, have conducted a detailed study to analyze the immune profiles of all those that had been infected with the SARS-CoV-2 coronavirus irrespective if they only had mild or moderate conditions.
https://www.thailandmedical.news/news/why-is-no-one-warning-the-masses-that-the-sars-cov-2-spike-proteins-are-causing-major-immunodeficiency-issues-in-all-infected-individuals
.jpg)
The study team from UNSW's Kirby Institute and St Vincent's Hospital Sydney alarmingly found that immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection and could even be longer!
This immune dysregulation could also be the reason for certain long COVID manifestations and could also lead to more serious long term medical and health conditions.
The study findings could also potentially pave the way for tailored treatment for those with ongoing symptoms.
To date it is already known that a large proportion of patients surviving acute coronavirus disease 2019 (COVID-19) infection develop Post-Acute Sequelae of SARS-CoV-2 infection (
PASC) or
Long COVID (LC) lasting longer than 12 weeks. At the same time, it is also coming to light now many who were eve asymptomatic or had mild to moderate symptoms upon SARS-CoV-2 infection are also developing Long COVID conditions. In fact from the initial estimations that around 33.3 percent of all who were infected with the SARS-CoV-2 virus irrespective if there were asymptomatic or symptomatic will develop one or more manifestations of Long COVID, the figure now has gone up to 87 percent based on both study and clinical data.
The Australian research team that have past extensive experience in HIV and immunology studied individuals with LC compared to age- and gender-matched recovered individuals without LC, unexposed donors and individuals infected with other coronaviruses.
The study findings showed that patients with LC had highly activated innate immune cells, lacked naive T and B cells and showed elevated expression of type I IFN (IFN-β) and type III IFN (IFN-λ1) that remained persistently high at 8 months after infection.
Utilizing a log-linear classification model, the study team defined an optimal set of analytes that had the strongest association with LC among the 28 analytes measured. Combinations of the inflammatory mediators IFN-β, PTX3, IFN-γ, IFN-λ2/3 and IL-6 associated with LC with 78.5–81.6% accuracy.
This study findings define immunological parameters associated with LC and suggests future opportunities for prevention and treatment.
The study findings were published in the peer reviewe
d journal: Nature Immunology.
https://www.nature.com/articles/s41590-021-01113-x
The study findings show that unvaccinated individuals with long COVID, even those whose initial infection was mild or moderate have a sustained inflammatory response for at least eight months following their infection, suggesting that long COVID is very different to other infections.
The study team used data obtained from St Vincent's Hospital's ADAPT study which collected samples from unvaccinated individuals during Australia's first pandemic wave.
Although evidence on long COVID has been accumulating through several clinical studies based on patient reporting, including the ADAPT Study, this is the first study to describe the impact of long COVID on the immune system through analysis in a laboratory setting.
Dr Chansavath Phetsouphanh, who is a senior research associate at the Kirby Institute and co-lead author on the paper told Thailand
Medical News, "Our study findings may validate some of the symptoms that individuals with long COVID experience. We found that there is a significant and sustained inflammation that indicates prolonged activation of the immune system response detectable for at least eight months following initial infection."
The study team examined blood samples from individuals with and without long COVID for a variety of 'immune biomarkers."
Dr Phetsouphanh added, "These are biological characteristics which can help us define a medical condition in an accurate and reproducible way. We compared these to individuals who had not had COVID-19, and we found persistently elevated levels of Type I and Type III interferons ie types of protein cells make in response to the presence of a virus. These interferons generally disappear after an infection clears, but in patients with long COVID we found they were present for an extended period."
Over at the the Kirby institute's specialized laboratories which are also used for HIV immunological studies, the study team analyzed multiple samples from 62 ADAPT patients diagnosed with COVID-19 between April and July 2020. Patient samples were analyzed at three, four and eight months following initial infection, and compared to control groups.
Dr Phetsouphanh added, "One of the most surprising aspects of our analysis is that individuals don't need to have had severe COVID to experience these ongoing immunological changes. This suggests that the pathophysiology ie that is the disordered physical processes associated with long COVID apply regardless of disease severity."
Lead author, Dr David Darley from St Vincent's Hospital says there is no data as to whether different variants like Omicron cause the same changes, or what role vaccination may play in reducing the risk of developing long COVID.
Dr Darley said, "From some early international data, we are very hopeful that with a milder variant and with high vaccination rates we may see less long COVID, but we will need further immunological data before we can say this for certain. We are currently looking at some data from the Delta wave to understand whether vaccination may reduce the possibility of long COVID."
The study team says that understanding the immune profile for long COVID will help the development of treatment and management of long COVID.
Professor Dr Anthony Kelleher, Director of the Kirby Institute commented, "This research provides the strongest evidence to date for a clear biological basis for the clinically apparent syndrome of long COVID. We will continue our analysis in response to the Omicron wave. In the meantime, with so many unknowns with both COVID and long COVID, we should do everything we can to reduce transmission."
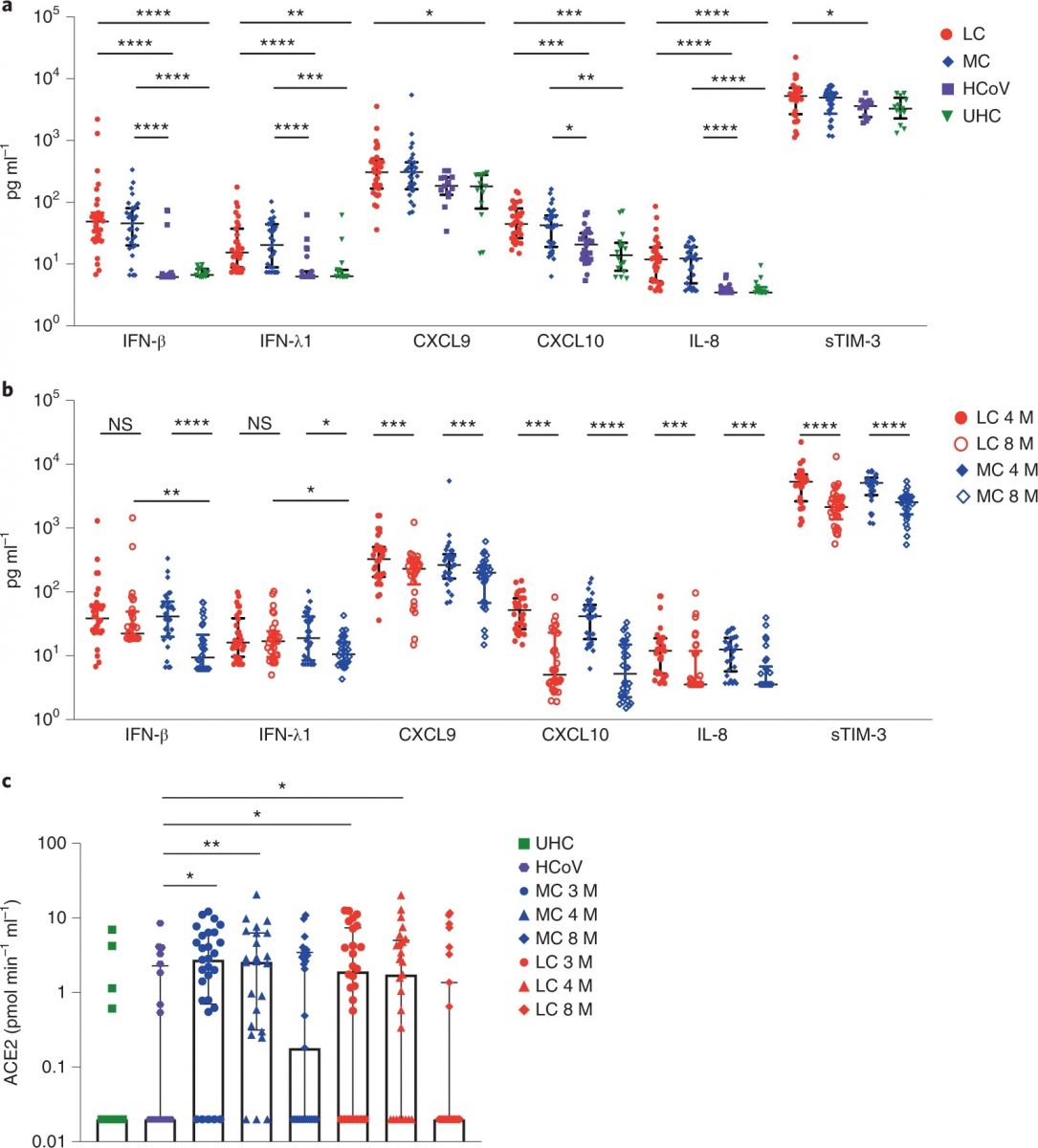 Higher levels of IFN-β, IFN-λ1, CXCL9, CXCL10, IL-8 and sTIM-3 at 4 months in the LC group (n = 31) and MC (n = 31) compared to individuals infected with common cold coronavirus (HCoV) (n = 25) and unexposed healthy donors (n = 13). b, Reduction of cytokine levels at 8 months. IFN-β and IFN-λ1 levels were higher in the LC group than the MC group at month 8. c, ACE2 activity increased at months 3 and 4 after SARS-CoV-2 infection and then decreased at 8 months in both groups. ACE2 activity in the HCoV and unexposed healthy donors (UHC) groups was minimal. Data are shown as medians with error bars representing interquartile ranges (IQRs). Kruskal–Wallis with Dunn’s correction was used for the 4-month analysis; two-tailed P values <0.05 (*), <0.01 (**), <0.001 (***) and <0.0001 (****) were considered significant. A Wilcoxon t test was used for paired comparison of 4- and 8-month data, and a Mann–
Higher levels of IFN-β, IFN-λ1, CXCL9, CXCL10, IL-8 and sTIM-3 at 4 months in the LC group (n = 31) and MC (n = 31) compared to individuals infected with common cold coronavirus (HCoV) (n = 25) and unexposed healthy donors (n = 13). b, Reduction of cytokine levels at 8 months. IFN-β and IFN-λ1 levels were higher in the LC group than the MC group at month 8. c, ACE2 activity increased at months 3 and 4 after SARS-CoV-2 infection and then decreased at 8 months in both groups. ACE2 activity in the HCoV and unexposed healthy donors (UHC) groups was minimal. Data are shown as medians with error bars representing interquartile ranges (IQRs). Kruskal–Wallis with Dunn’s correction was used for the 4-month analysis; two-tailed P values <0.05 (*), <0.01 (**), <0.001 (***) and <0.0001 (****) were considered significant. A Wilcoxon t test was used for paired comparison of 4- and 8-month data, and a Mann–
Typically, when scientists screen blood samples to understand an infection or immune response to an infection, there are hundreds of different markers that they could potentially look for to help them analyze exactly what the disease is doing to the body.
Dr Phetsouphanh explained, "As immunologists we're almost like detectives at a crime scene. We have thousands of potential biomarkers or ‘leads’ to investigate, but only a handful of them will reveal something useful. We can use some of our knowledge of what's been measured in acute COVID and other post-viral fatigue syndromes to narrow the investigation down a little bit, but because long COVID is still a new syndrome, we have to take a broad examination of the evidence and look almost everywhere."
He further added, "In conducting this research, we were looking for proteins in the serum. These proteins, or biomarkers, are evidence of an abnormal process caused by a disease. We analyzed 31 different biomarkers that we suspected could be 'triggered' by COVID-19, and we identified a small subset that were associated with long COVID syndrome. Excitingly, by looking at subsets of cells within the immune system we found the possible site of production of these biomarkers, which could be crucial for developing treatments."
Ms Doris Gal from Shellharbour, who is part of the ADAPT study and had tested positive for COVID in September 2020 said, "COVID is the virus that keeps on giving. My initial infection was quite mild, however my long COVID symptoms are significant. I've lost the ability to comprehend the way I did before having COVID. I used to be a PA, but I can't do that job anymore. Hearing about this research, I feel like my symptoms have been validated."
It was reported that approximately 30 percent of unvaccinated individuals who contracted COVID and were followed in the ADAPT study have experienced some long COVID symptoms.
Mr Rick Walters from Roseville contracted COVID in August 2020 and is part of the ADAPT study. He is experiencing long COVID symptoms, and he says the findings raise mixed emotions. He said, "I'm glad that the study has confirmed that long COVID is a valid result of COVID-19 infection and just not something in my head. At first, I thought I would get better, but it became apparent that the damage to my lung was permanent, and I became quite anxious.I have had some difficulties adjusting to my current health. COVID should not be taken lightly. I am gradually learning to live with the results."
Professor Dr Gail Matthews co-leads ADAPT and is Head of Infectious Diseases at St Vincent's Hospital and Program Head of Vaccine and Therapeutic Research at the Kirby Institute. She says when someone has a virus, the immune system gets switched on to respond to the virus and eliminate it.
Professor Matthews added, "But what we're seeing with long COVID is that even when the virus has completely left the body, the immune system remains switched on. If you measure the same thing after a standard cough or cold, which we did in this study through one of our control groups, this signal is not there. It's unique to sufferers of long COVID."
Professor Matthews says that through research like this we are slowly starting to understand some of the mysteries of long COVID.
She added, "Simply put, when we look carefully at the immune system in people who have had COVID-19 infection, and particularly at those with long COVID, it looks different to what we would expect in healthy individuals. This tells us that there might be something quite unique in the pathophysiology of this disease. The next steps are to apply this new understanding to other COVID-19 variants, and to further research to inform the treatment and management of long COVID."
Thailand Medical News would like to add that while the study importantly shows that the SARS-CoV-2 virus dysregulates the immune system for a long time, it is not the only cause of Long COVID. Many other studies are now showing that a variety of factors are responsible for Long COVID as the SARS-CoV-2 has a variety of ways directly or indirectly to affect the various human host cellular pathways, tissues and organs. One study has shown that viral persistence is real and could also be another contributing factor to Long COVID.
https://www.thailandmedical.news/news/breaking-u-s-nih-study-shockingly-reveals-sars-cov-2-viral-persistence-throughout-human-body-and-in-the-brain-even-in-those-who-were-asymptomatic
For the latest on
Long COVID, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-mutations-on-omicron-non-structural-protein-6-nsp6-alters-viral-disruption-modes-of-autophagy-in-host,-leading-to-possibly-more-serious-long-
https://www.thailandmedical.news/news/breaking-sars-cov-2-infection-induces-increase-of-gp73-that-causes-dysglycaemia-increased-gp73-could-also-imply-future-liver-disease-and-liver-cancer
https://www.thailandmedical.news/news/great-news-south-korean-study-shows-that-sars-cov-2-is-literally-killing-the-microglia-cells-in-the-host-brain-hence-the-various-arising-neurological-
https://www.thailandmedical.news/news/more-great-news-stanford-yale-study-shows-even-mild-sars-cov-2-infection-can-cause-multi-lineage-cellular-dysregulation-and-myelin-loss-in-the-brain
https://www.thailandmedical.news/news/more-great-news-stanford-yale-study-shows-even-mild-sars-cov-2-infection-can-cause-multi-lineage-cellular-dysregulation-and-myelin-loss-in-the-brain
https://www.thailandmedical.news/news/german-study-shockingly-discovers-that-sars-cov-2-caused-complement-activation-induces-excessive-cd16-t-cells-with-increased-cytotoxic-functions
For more on
long COVID, go to:
https://www.thailandmedical.news/articles/long-covid
.jpg)
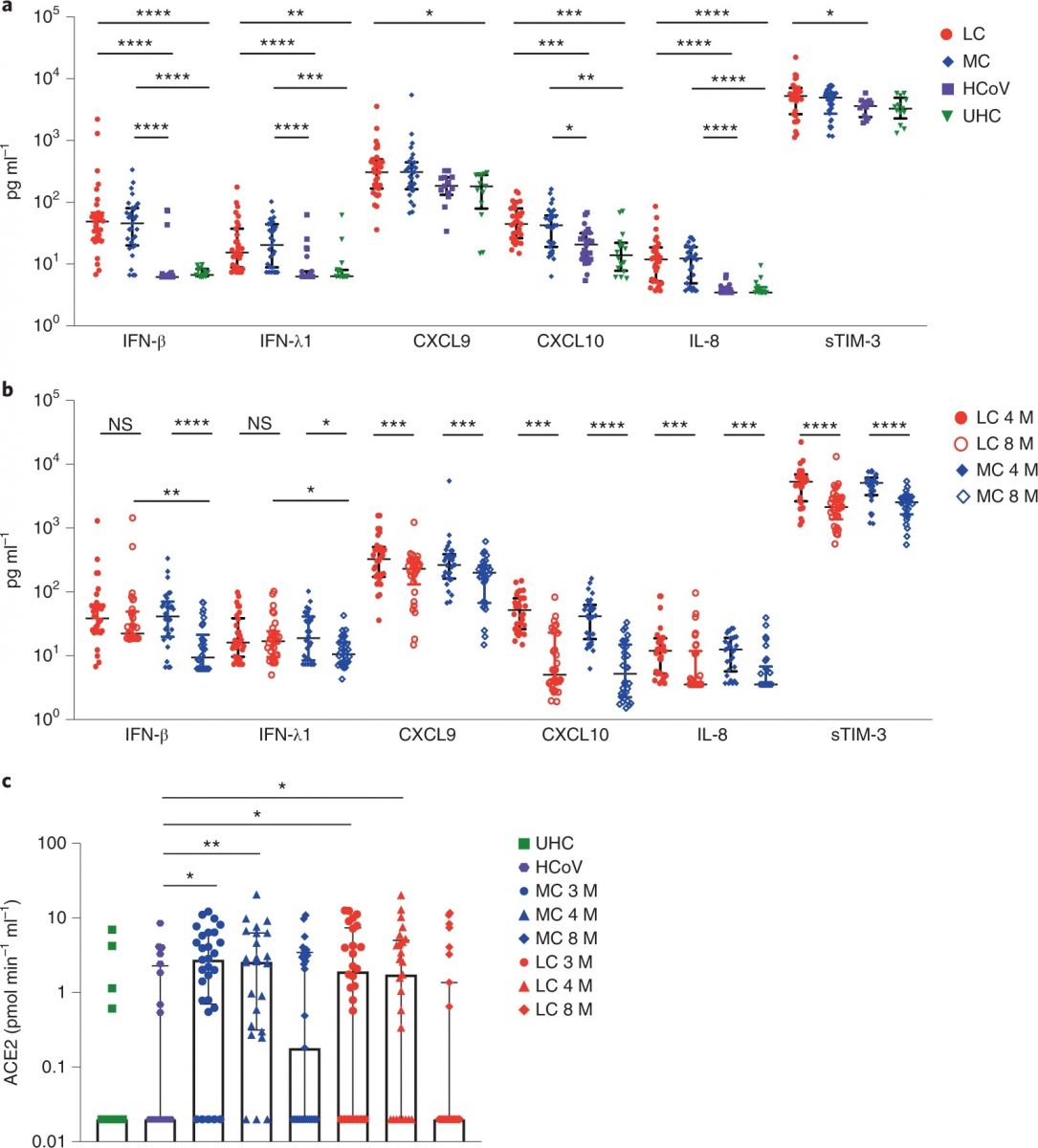 Higher levels of IFN-β, IFN-λ1, CXCL9, CXCL10, IL-8 and sTIM-3 at 4 months in the LC group (n = 31) and MC (n = 31) compared to individuals infected with common cold coronavirus (HCoV) (n = 25) and unexposed healthy donors (n = 13). b, Reduction of cytokine levels at 8 months. IFN-β and IFN-λ1 levels were higher in the LC group than the MC group at month 8. c, ACE2 activity increased at months 3 and 4 after SARS-CoV-2 infection and then decreased at 8 months in both groups. ACE2 activity in the HCoV and unexposed healthy donors (UHC) groups was minimal. Data are shown as medians with error bars representing interquartile ranges (IQRs). Kruskal–Wallis with Dunn’s correction was used for the 4-month analysis; two-tailed P values <0.05 (*), <0.01 (**), <0.001 (***) and <0.0001 (****) were considered significant. A Wilcoxon t test was used for paired comparison of 4- and 8-month data, and a Mann–
Higher levels of IFN-β, IFN-λ1, CXCL9, CXCL10, IL-8 and sTIM-3 at 4 months in the LC group (n = 31) and MC (n = 31) compared to individuals infected with common cold coronavirus (HCoV) (n = 25) and unexposed healthy donors (n = 13). b, Reduction of cytokine levels at 8 months. IFN-β and IFN-λ1 levels were higher in the LC group than the MC group at month 8. c, ACE2 activity increased at months 3 and 4 after SARS-CoV-2 infection and then decreased at 8 months in both groups. ACE2 activity in the HCoV and unexposed healthy donors (UHC) groups was minimal. Data are shown as medians with error bars representing interquartile ranges (IQRs). Kruskal–Wallis with Dunn’s correction was used for the 4-month analysis; two-tailed P values <0.05 (*), <0.01 (**), <0.001 (***) and <0.0001 (****) were considered significant. A Wilcoxon t test was used for paired comparison of 4- and 8-month data, and a Mann–