Low Muscle Mass Can Increase Risk Of Health Conditions And Lower Survival Rates Of Those Sick
Source: Thailand Medical News Jan 12, 2020 5 years, 3 months, 2 weeks, 12 hours, 52 minutes ago
Following diets that lead to
weigh loss might not always result in better health, especailly if you lose
muscle mass. Sedentary lifestyles and age also leads to
muscle mass loss can lead to a wide range of chronic illnesses or even aggravate current health conditions.
Diet and nutrition expert Dr Carla Prado has written extensively about the dangers of low
muscle mass across a wide range of body types. According to her recent review of nearly 150 studies published over a single year, patients with low muscle mass experience more complications, longer hospital stays and lower survival rates.
Dr Prado told
Thailand Medical News, "
Muscle is very important for movement and balance, for posture, strength and power, but it's also a reservoir of amino acids. The more you lose, the greater the consequences."
Dr Prado in a new study, argues that nutrition interventions could improve
cancer treatment, making a high-protein, high-nutrient diet a crucial tool in the fight against a life-threatening illness.
Some critics have long suggested the
body mass index—a simple calculation of weight over height, glosses over important differences in body types. A sedentary wrestling fan might have a normal
BMI, while a big size boxer could likely qualify as obese.
Dr Prado likes to compare oranges and pomelos, citrus fruits with very different peel-to-fruit ratios.
Dr Prado explained, "You can have people that have exactly the same body weight,". "On the scale they look the same. But when you look at their
body composition, the amount of
muscle is very different."
A few years ago, researchers began noticing an "obesity paradox" among patients with chronic diseases. Higher
BMI patients often fared better than low
BMI patients. While researchers puzzled over why that could be, Prado believes the answer actually lies beneath the surface. It's the
muscle, she argues, not the fat.
At University of Alberta’s Human Nutrition Research Unit, where Dr Prado is the director, she is still building on work she began a decade ago as a Ph.D. student. Looking at
muscle mass and
cancer outcomes, she had difficulty finding thin patients with low
muscle mass. She focused on
cancer patients with obesity instead.
That research work led to a groundbreaking study in
The Lancet Oncology that linked outcomes to
muscle mass, a paper that's been cited nearly 1,000 times since its 2008 publication.
Dr Prado, who became a University of Alberta faculty member five years ago, believes body composition research has massive implications for the way chronic d
iseases are treated. Chemotherapy, for example, is often administered based on body weight, leaving patients with obesity and low
muscle mass at a higher risk of toxicity. But she also thinks nutrition has the potential to transform care simply by focusing on maintaining and building muscle.
A chronic illness is like a wildfire, Prado said, devastating a body's
muscle reservoir at a rapid rate. That lost
muscle (sarcopenia) has many important roles beyond mobility, including regulating hormones, metabolic functions and organ function.
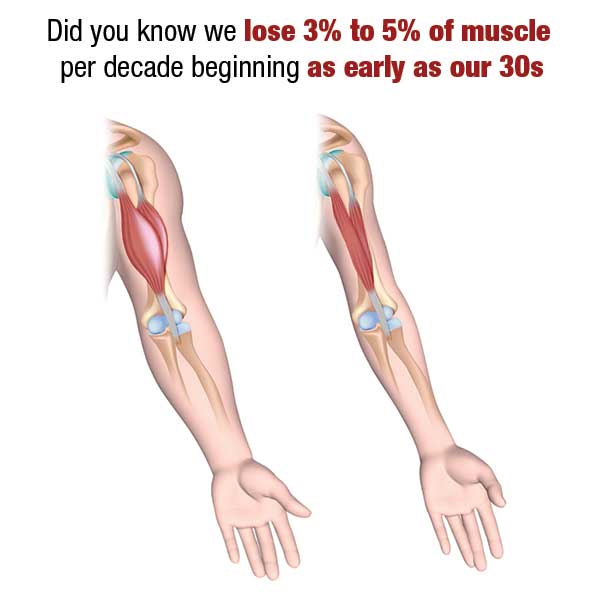
In 72 hours, an elderly patient in a hospital bed, can lose more than a kilogram of
muscle while over a 10-day hospital stay, a healthy adult can lose five percent of their total
muscle mass. Those numbers rise to 18 percent in an intensive care unit.
Dr Prado added, "You can lose it so fast, but rebuilding it takes months. Can you imagine one kilo, trying to put that on in a week or so? It's almost impossible."
Muscle deterioration makes it harder to fight illness. A 10 percent loss leads to impaired immunity and increased risk of infection. Twenty percent means weakness and slowed healing; 30 percent leaves a patient too weak to sit. A loss of 40 percent is often fatal.
Also there are other things to consider. With worse outcomes, additional complications and longer hospital stays, ignoring
muscle mass costs health systems more resources. Prado said patients end up with a poorer quality of life, unable to perform the most basic tasks like opening a bottle of water or combing their hair.
Dr Prado is looking at how dietary interventions could be used to prevent or treat diseases by building
muscle, once again returning to
cancer. While food guidelines are often "one size fits all," Prado believes increasing protein and
muscle-building nutrients could radically improve outcomes. Nutrition should be considered a therapy.
She added, "We take nutrition for granted, but it's truly important. Just like we need oxygen to breathe, our
muscles need protein and amino acids to grow."
A new wide range of studies have suggested new metrics that better capture health than
BMI:
body composition, walking speed, grip strength or the ability to do push-ups. Irrespective of how
muscle mass is measured, Prado thinks it needs to be a new vital sign. Doctors should be asking patients whether they have problems getting out of their car, she said. And patients facing a disease should be asking doctors how their body composition could affect treatment.
She added, "Every other medical field has evolved into using sophisticated techniques, so why would dietitians rely on something Hippocrates could have done. We have to evolve."
Dr Prado wants to take the focus off of the bathroom scale and continue looking deeper. Adding
muscle or at least retaining it could truly mean an ounce of prevention is better than a pound of cure.
Reference : Carla MM Prado et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study, The Lancet Oncology (2008). DOI: 10.1016/S1470-2045(08)70153-0