Source: Michigan Medicine Jul 16, 2018 6 years, 9 months, 1 week, 6 days, 10 hours, 43 minutes ago
New Research finds that more men have suboptimal testosterone levels than previously known, and it may be putting these men at risk. Testosterone hormone replacement therapy is great tool in preventing diseases associated with aging in men.
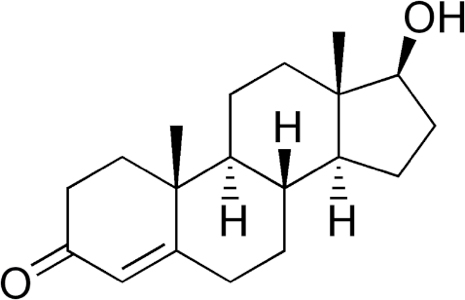
A male’s total testosterone level may be linked to more than just sexual health and muscle mass preservation, a new study finds. Low amounts of the hormone could also be associated with chronic disease, even among men 40 years of age and younger.
“If we look at data for men from a population level, it has become evident over time that chronic disease is on the rise in older males,” says Mark Peterson, Ph.D., M.S., FACSM, lead author of the study and assistant professor of physical medicine and rehabilitation at Michigan Medicine. “But we’re also finding that a consequence of being obese and physically inactive is that men are seeing declines in testosterone even at younger ages.”
Published in Scientific Reports, Peterson and colleagues studied this relationship among testosterone, age and chronic disease.
“Previous research in the field has shown that total testosterone deficiency in men increases with age, and studies have shown that testosterone deficiency is also associated with obesity-related chronic diseases,” Peterson says. “But it hasn’t been previously understood what the optimal levels of total testosterone should be in men at varying ages, and to what effect those varying levels of the hormone have on disease risk across the life span.”
The study’s basis came from previous work from other researchers that appeared to define normal ranges of testosterone but didn’t use population-representative cohorts, he says.
“Previous studies used clinical cohorts that were not reflective of the current male population in the United States,” Peterson says. “The cohorts they used enforced strict guidelines for patients that were accepted into the cohort. Therefore, those patients tended to be much healthier.”
Peterson and colleagues, then, leveraged a population sample that was much more representative of males in the United States today.
Multimorbidity across age groups
Using data from the National Health and Nutrition Examination Survey, the research team examined the extent to which hypogonadism is prevalent among men of all ages.
Of the 2,399 men in the survey who were at least 20 years old, 2,161 had complete information on demographics (e.g., age, ethnicity and household income), chronic disease diagnoses, blood samples obtained for total testosterone, grip strength and lab results for cardiometabolic disease risk factors.
Peterson and team then examined prevalence of nine chronic conditions, including
type 2 diabetes, arthritis, cardiovascular disease, stroke, pulmonary disease, high triglycerides, hypercholesterolemia, hypertension and clinical depression.
The researchers studied the prevalence of multimorbidity, or when two or more of the chronic conditions were present, among three age groups (young, middle-aged and older men) with and without testosterone deficiency. They found that low total testosterone was associated
with multimorbidity in all age groups — but it was more prevalent among young and older men with testosterone deficiency.
“We also found a large dose-response relationship between the age-specific low total testosterone and moderate total testosterone levels and multimorbidity, even after adjusting for obesity and muscle strength capacity,” Peterson says. “Which means that men should be concerned about declining total testosterone, even if it has not reached a level to warrant a clinical diagnosis (<300 ng/dL [10.4 nmol/L]).”
Co-author Aleksandr Belakovskiy, M.D., a resident in family medicine at Michigan Medicine, who helped to design and carry out the study, notes that the results show the need for further testing and research.
“This study showed a robust association between testosterone and multiple medical morbidities that could influence the way we think about testosterone in general practice,” Belakovskiy says. “While these findings cannot prove causation, it does spark the need for better clinical awareness and more research.”
The team hopes the study and its results can serve as a public service announcement for men.
“A lot of men may not be aware of the risk factors for testosterone deficiency because of their current lifestyle,” Peterson says. “And more importantly, that declining levels could be contributing to a silent decline in
overall health and increased risk for chronic disease.”
Reference: Michigan Medicine