Medical Thailand: Thai Study Validates That COVID-19 Induced Immune Dysfunction Is Driving Increased Incidence Of Pulmonary Tuberculosis!
COVID-19 News - Pulmonary Tuberculosis in Post COVID Feb 01, 2023 2 years, 2 months, 3 weeks, 5 days, 20 hours, 20 minutes ago
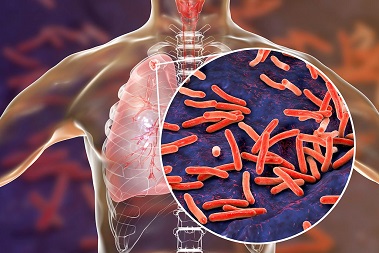
Medical Thailand: Researchers from the Department of Epidemiology, Faculty of Medicine, Prince of Songkhla University-Thailand have in a new study validated that there is an increased incidence of detecting pulmonary tuberculosis (PTB) in patients hospitalized with COVID-19 pneumonia compared with that in the general population.
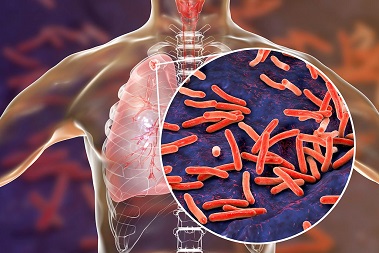
The study findings shockingly showed that the cumulative incidence of PTB among patients with SARS-CoV-2 infection was steep at ten-fold of the population control in the early period (within 30 days after infection), and it declined to six-fold thereafter.
A previous South African hospital-based study reported a 3-fold increase in the incidence of pulmonary tuberculosis (PTB) in those previously inflicted with COVID-19 pneumonia compared with that in the general population.
https://pubmed.ncbi.nlm.nih.gov/35725387/
It is well known that tuberculosis (TB) infection (TBI) can progress to active TB disease after an immunosuppressive event.
Numerous studies have already shown that patients with COVID-19 have decreased levels of functional T-cells during the illness period causing immune dysfunction. In practice, this depletion of immunity or immune dysfunctional state can lead to an increased incidence of active TB in populations with a high TB prevalence.
In our previous past
Medical Thailand News coverages, we have covered about how SARS-CoV-2 infections causes COVID-19 induced immune dysfunction and COVID-19 induced immunodeficiency.
https://www.thailandmedical.news/news/why-is-no-one-warning-the-masses-that-the-sars-cov-2-spike-proteins-are-causing-major-immunodeficiency-issues-in-all-infected-individuals
https://www.thailandmedical.news/news/long-covid-news-australian-study-shows-that-immune-dysfunction-persists-for-up-to-8-months-after-initial-mild-or-moderate-sars-cov-2-infection
https://www.thailandmedical.news/news/breaking-italian-study-validates-previous-claims-that-sars-cov-2-infections-causes-immunodeficiency-conditions-worse-than-hiv-infections
https://www.thailandmedical.news/news/covid-19-news-germany-s-health-minister-warns-that-exposure-to-sars-cov-2-will-result-in-an-incurable-immunodeficiency-condition
The Thai study team aimed to estimate the risk of having detec
table active PTB after SARS-CoV-2 infection.
The researchers utilized data from Insurance claims in lower Southern Thailand from the 12th regional National Health Security Office, Thailand. Inpatient and outpatient electronic medical records were linked using encrypted identification numbers. Records of individuals aged ≥18 years from 1 April to 30 September 2021 were retrieved to form a dynamic cohort. Exposure status was based on SARS-CoV-2 investigation and pneumonia status: population control (general population who had never been tested), negative reverse transcription-polymerase chain reaction (RT-PCR) control, asymptomatic COVID-19, symptomatic COVID-19 without pneumonia, and COVID-19 pneumonia groups. They were tracked in the databases for subsequent bacteriologically confirmed PTB until 31 March 2022.
A total of 4,241,201 individuals were recruited in the dynamic cohort and contributed 3,108,224, 227,918, 34,251, 10,325, and 14,160 person-years in the above exposure groups, respectively. Time-varying Cox's regression was conducted using population control as reference.
The study findings showed hazard ratios (95% CIs) of the negative control, asymptomatic, symptomatic COVID-19 without pneumonia, and pneumonia groups were 1.58 (1.08, 2.32), 1.00 (0.25, 4.01), 2.98 (0.74, 11.98), 9.87 (5.64, 17.30) in the first 30 days and 0.97 (0.81, 1.15), 1.41 (0.92, 2.17), 3.85 (2.42, 6.13), and 7.15 (5.54, 9.22) thereafter, respectively.
The study findings validated previous findings that having had COVID-19 pneumonia, as opposed to the general population status, was strongly associated with a higher hazard of detectable active PTB.
The study team suggested that in tuberculosis endemic areas, patients with COVID-19 pneumonia should be closely followed up to reduce PTB-related burden.
The study findings were published in the peer reviewed journal: eClinical Medicine (Lancet Discovery Science).
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00002-0/fulltext
TB or Tuberculosis, a critical global infectious disease (GID), has been superimposed by the COVID-19 pandemic since 2020.
According to the study team, In low- and middle-income countries (LMICs), information about the risk of getting active pulmonary tuberculosis (PTB) would guide health programs on active surveillance of TB among post-COVID-19 patients.
Typically, the spectrum of PTB starts from tuberculosis infection (TBI), which is not contagious (dormant bacilli),to subclinical PTB with undetectable or detectable bacilli, and ends in active PTB with signs and symptoms, in which the bacilli are detected.
In countries like Thailand, subclinical PTB is often coincidentally detected during investigations for other purposes, and clinically active PTB patients visit healthcare centers because of signs and symptoms.
It has been found that COVID-19 pneumonia usually causes excessive cellular immune responses, resulting in functional exhaustion and T-cell depletion, which can increase the risks of progression from TBI to active PTB.
https://pubmed.ncbi.nlm.nih.gov/27601645/
https://pubmed.ncbi.nlm.nih.gov/22480184/
https://www.sciencedirect.com/science/article/pii/S1201971219300992
https://pubmed.ncbi.nlm.nih.gov/31054408/
https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1005687
Past studies in China asserted that there is a significantly decreased number of CD8+ cells at the time of SARS-CoV-2 infection.
https://pubmed.ncbi.nlm.nih.gov/32425950/
https://pubmed.ncbi.nlm.nih.gov/32574709/
Also, the depletion of CD4+ and CD8+ in the early period of the SARS-CoV-2 infection has a dose–response relationship with the severity of COVID-19.
https://pubmed.ncbi.nlm.nih.gov/32425950/
https://pubmed.ncbi.nlm.nih.gov/32574709/
Hence, the severity of COVID-19 could be a surrogate variable for the T-cell count affecting clinical presentation.
Another study in China reported that 73.6% of patients with pneumonia could recover their T-cell numbers within approximately 30 days, whereas the remaining 26.4% had prolonged T-cell depletion.
https://pubmed.ncbi.nlm.nih.gov/33240994/
It was noted that decreased cellular immune response due to T-cell depletion could mediate the increased risk of getting active TB.
The study findings shockingly showed that the cumulative incidence of PTB among patients with SARS-CoV-2 infection was steep at ten-fold of the population control in the early period (within 30 days after infection), and it declined to six-fold thereafter.
Interestingly, in the second period, patients with symptomatic COVID-19 (both with pneumonia and without pneumonia) demonstrated an increased hazard of detectable active PTB.
The study findings could explain why patients with COVID-19 pneumonia may be at increased risk of subsequent PTB even if their COVID-19 symptoms are cured.
It is hypothesized that while SARS-CoV-2 is different from TB, it probably weakens individuals with TB infection and accelerates their progression toward active PTB.
In the current study, patients with PTB were diagnosed after being discharged from the hospital in the median of 175 days. They were more likely to have active PTB during their post-COVID-19 period.
The study's strength is the completeness of COVID-19 and PTB diagnoses data based on a large population by the law for reimbursement that was followed up for at least 180 days.
The major biological risk factors for PTB, i.e., age, sex, HIV infection, DM, cancers, and COPD, were already controlled for. Thus, they could not explain this independent association between COVID-19 and PTB.
The study team in conclusion, suggest that individuals who recently survived COVID-19 pneumonia in a TB endemic area should receive special attention regarding the robust association between COVID-19 pneumonia and the hazard of detectable active PTB.
More detailed studies are warranted on this population on TB infection and the cost-utility for screening and TB preventive therapy are needed.
The study team also stressed that patients with subclinical PTB or active PTB have a higher chance of being detected if they have a positive test for SARS-CoV-2 infection and are hospitalized.
For the latest
Medical Thailand News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-warnings-sars-cov-2-coronavirus--infection-could-activate-dormant-tuberculosis
https://www.thailandmedical.news/news/breaking-turkey-medical-researchers-based-on-actual-clinical-case-reports-warn-that-covid-19-is-reactivating-dormant-tuberculosis-in-individuals-inclu
https://www.thailandmedical.news/news/ohio-state-university-murine-study-surprisingly-discovers-that-tuberculosis-infection-induces-resistance-to-secondary-covid-19