Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 02, 2024 6 months, 1 week, 4 days, 1 hour, 55 minutes ago
Medical News: A recent medical report from Shanghai Xuhui Central Hospital in China has uncovered a rare yet critical case of branch retinal artery occlusion (BRAO) in a 76-year-old man, potentially linked to a mild COVID-19 infection. This condition, which led to sudden vision loss in the patient's left eye, involved three retinal arteries and has been attributed to elevated levels of inflammatory markers and coagulation factors - both common issues seen in COVID-19 cases.
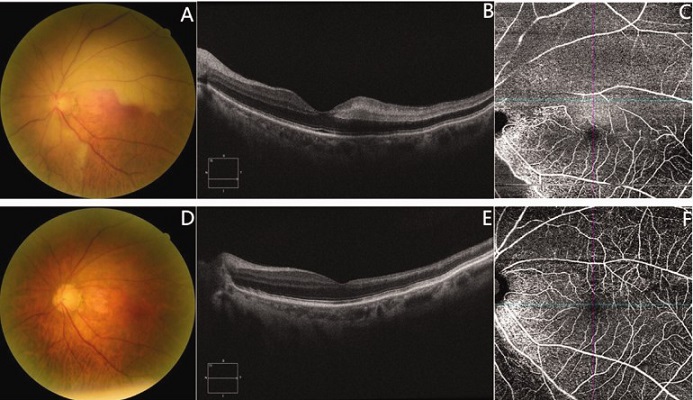
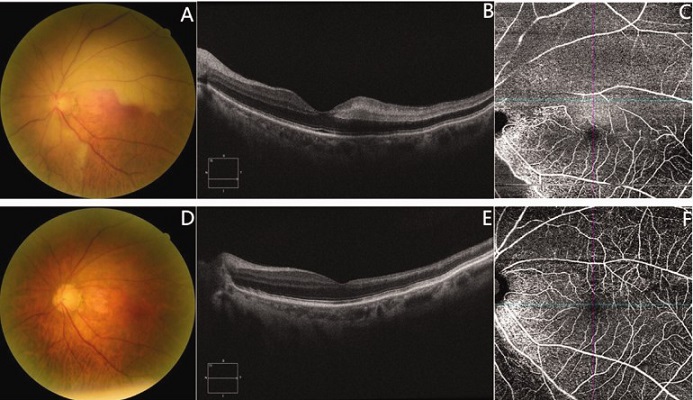 Colour fundus images from optical coherence tomography (OCT), and optical coherence tomography angiography (OCTA) of the patient’s left eye at presentation (a–c) and 25 days after starting treatment (d–f). (a) Fundus image showing an extremely fine arterial diameter, with grey-white oedema in the supranasal, infranasal, and supratemporal quadrants that involved the fovea. (b) Macular OCT showing diffuse signal enhancement in the inner layer of the foveal temporal side retina. (c) En- face OCTA showing the loss of superficial capillaries in the supranasal, infranasal and supratemporal quadrants. (d) Fundus image taken 25 days after starting treatment showing the normal colour of the retina. (e) Macular OCT taken 25 days later showing atrophy and thinning of the foveal temporal side retina and (f) en-face OCTA taken 25 days later showing recovery of the superficial capillaries in the supranasal, infranasal and supratemporal quadrants.
Colour fundus images from optical coherence tomography (OCT), and optical coherence tomography angiography (OCTA) of the patient’s left eye at presentation (a–c) and 25 days after starting treatment (d–f). (a) Fundus image showing an extremely fine arterial diameter, with grey-white oedema in the supranasal, infranasal, and supratemporal quadrants that involved the fovea. (b) Macular OCT showing diffuse signal enhancement in the inner layer of the foveal temporal side retina. (c) En- face OCTA showing the loss of superficial capillaries in the supranasal, infranasal and supratemporal quadrants. (d) Fundus image taken 25 days after starting treatment showing the normal colour of the retina. (e) Macular OCT taken 25 days later showing atrophy and thinning of the foveal temporal side retina and (f) en-face OCTA taken 25 days later showing recovery of the superficial capillaries in the supranasal, infranasal and supratemporal quadrants.
Despite underlying conditions like hypertension, the case stands out as an example of how COVID-19 can affect parts of the body beyond the respiratory system. This
Medical News report delves into the details of the case, its treatment, and the potential connection between COVID-19 and retinal artery blockages.
Background on Retinal Artery Occlusion and COVID-19
COVID-19, the global pandemic that primarily affects the respiratory system, has been associated with several complications in various organs, including the gastrointestinal tract, heart, and blood vessels. One of the critical mechanisms behind these complications is the infamous "cytokine storm," which can lead to inflammation and hypercoagulation, contributing to blood clots and vascular damage. While respiratory and cardiovascular issues are more commonly discussed, the case of BRAO highlights the risk of less frequent complications, such as retinal artery occlusion.
Retinal artery occlusions are considered rare in patients, but their occurrence in individuals recovering from or infected by COVID-19 has drawn attention in recent medical literature. This article sheds light on one such case where a patient’s visual function significantly improved following a series of treatments, including anti-inflammatory, anticoagulant, and conservative therapies.
Case Presentation
In January 2023, a 76-year-old man arrived at Shanghai Xuhui Central Hospital’s outpatient department after experiencing sudden vision impairment and a dark shadow obstructing his left eye. The symptoms had persisted for two days. The patient had no known history of diabetes or high cholesterol but had been living with
hypertension for five years, which was well-managed with medication.
Prior to his eye issue, the patient experienced a dry cough and fever in late December 2022 and tested positive for COVID-19 through a reverse transcription polymerase chain reaction (RT-PCR) test. His symptoms subsided within a few days without the need for medication, and he tested negative for COVID-19 by the end of the month. At the time of his visit for the eye problem, the patient's blood pressure was normal, and his temperature had returned to normal as well.
Upon examination, his corrected visual acuity for the left eye was measured at 6/20, while the right eye remained at 20/20. A thorough examination of his left eye revealed a narrowed arterial diameter and grey-white edema across various quadrants of the eye. Macular optical coherence tomography (OCT) showed signal enhancement in parts of the retina, and further tests confirmed significant damage to the superficial capillaries in the affected areas.
Laboratory Findings and Diagnosis
The patient’s blood work revealed elevated levels of inflammatory and coagulation markers, including interleukin-6 (IL-6), C-reactive protein (CRP), and D-dimer, all of which are linked to inflammation and clotting. Additionally, his erythrocyte sedimentation rate (ESR) and fibrinogen levels were higher than normal, signaling a hypercoagulable state that is often observed in COVID-19 patients. His blood oxygen saturation was slightly low at 94%, further indicating systemic issues.
The patient was diagnosed with branch retinal artery occlusion (BRAO) related to his recent COVID-19 infection, based on these findings. Although he had a history of hypertension, his condition had been stable and well-controlled, suggesting that COVID-19 may have exacerbated his vascular risks.
Treatment and Recovery
The patient was immediately admitted to the hospital, where doctors implemented a range of treatments to address his eye condition. This included anti-inflammatory treatment with prednisone, anticoagulation therapy with aspirin, and supplemental oxygen. Additionally, the patient received vasodilation treatment through retrobulbar injections and isosorbide nitrate infusions to improve blood flow to the retina. Nine days after initiating treatment, his inflammatory markers had decreased significantly, with IL-6 levels returning to normal. His D-dimer and fibrinogen levels had also decreased, indicating a reduction in his body’s procoagulant state.
Twenty-five days after starting treatment, the patient's visual acuity in his left eye had returned to 20/20, and the retinal edema had resolved. Imaging tests confirmed that the damaged superficial capillaries had largely recovered, although some residual defects in his visual field remained. Despite the overall improvement, these remaining defects were likely due to reduced oxygen saturation levels during the acute phase of his illness, which left lasting damage to parts of the retina.
Implications and Discussion
This case highlights a critical yet underexplored aspect of COVID-19: its potential to cause vascular complications beyond the lungs and heart. Retinal artery occlusions, while rare, have been reported in COVID-19 patients, particularly those with elevated inflammatory and coagulation markers. The fact that the patient in this case recovered most of his visual function after targeted treatments is a testament to the importance of early diagnosis and intervention.
The underlying mechanisms that may link COVID-19 to retinal artery occlusion are still not fully understood, but they likely involve the downregulation of angiotensin-converting enzyme 2 (ACE2) in retinal tissues. ACE2, which is also targeted by the SARS-CoV-2 virus, plays a key role in maintaining vascular health, and its suppression can lead to inflammation and clot formation. More research is needed to establish a definitive link between COVID-19 and retinal vascular occlusion, but the evidence from this case and others suggests that COVID-19 patients may be at increased risk of these complications.
Conclusion
In this report, we described a patient with branch retinal artery occlusion (BRAO) involving three arteries, which appeared to be related to a recent mild COVID-19 infection. The patient’s elevated inflammatory and coagulation markers pointed to a possible systemic effect of the virus, leading to vascular complications. Following treatment with anti-inflammatory, anticoagulant, and conservative therapies, the patient’s vision improved significantly, although some visual defects remained. This case emphasizes the importance of recognizing the potential for COVID-19 to cause complications beyond the respiratory system, especially in patients with underlying vascular risk factors. Early diagnosis and intervention are crucial for improving outcomes in such cases.
The study findings were published in the peer-reviewed Journal of International Medical Research.
https://journals.sagepub.com/doi/full/10.1177/03000605241284931
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-even-mild-covid-19-can-cause-microvasculature-changes-of-the-optic-nerve
https://www.thailandmedical.news/news/covid-19-s-hidden-impact-on-eyes-unveiling-rare-retinal-conditions