Mites That Cause Scabies Are Now Evolving To Evade Standard Treatments Involving Permethrin!
Scabies - Permethrin Resistance Apr 25, 2023 1 year, 11 months, 2 weeks, 6 days, 13 hours, 56 minutes ago
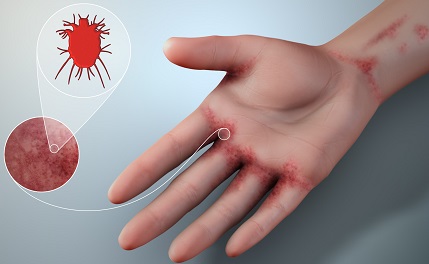
Scabies, a highly contagious parasitic skin disease caused by the Sarcoptes scabiei var. hominis mite, has plagued humanity for centuries. It affects people of all ages and socio-economic backgrounds, with an estimated 200 million cases reported globally each year.
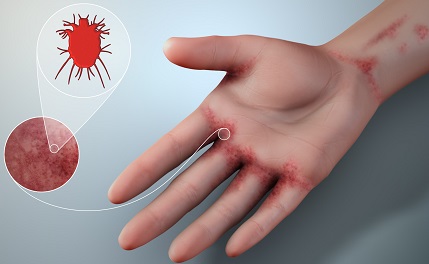
The most common treatment for
scabies, a topical insecticide called permethrin, has been the gold standard for decades. However, recent studies have identified the emergence of permethrin-resistant scabies, raising concerns about the future efficacy of this treatment and the need for alternative strategies.
The Emergence of Permethrin Resistance
Permethrin, a synthetic pyrethroid, was first introduced in the 1970s as a broad-spectrum insecticide. It works by targeting the mite's nervous system, causing paralysis and eventual death. Permethrin has been highly effective in treating scabies and remains the first-line treatment in most parts of the world. However, recent studies have documented increasing cases of permethrin-resistant scabies, raising concerns for global public health.
One of the first studies to report permethrin resistance in scabies was an Australian study that reported a high permethrin treatment failure rate among indigenous communities in northern Australia. The study highlighted the need for ongoing surveillance and the development of alternative treatments.
https://www.futuremedicine.com/doi/abs/10.2217/17460913.3.1.57
A 2008 study by Pasay et al., published in medical and Veterinary Entomology provided further evidence of permethrin resistance in scabies. The study identified specific genetic mutations in the voltage-gated sodium channels of the mite's nervous system, which are associated with resistance to pyrethroid insecticides like permethrin. The authors also reported that the frequency of these mutations was significantly higher in permethrin-resistant mite populations.
https://resjournals.onlinelibrary.wiley.com/doi/10.1111/j.1365-2915.2008.00716.x
Mechanisms of Permethrin Resistance
The exact mechanisms of permethrin resistance in scabies remain under investigation. However, studies suggest that multiple factors contribute to the development of resistance. These include:
-Target-site insensitivity: Genetic mutations in the mite's nervous system, particularly in the voltage-gated sodium channels, can render permethrin less effective in binding to its target sites. This leads to a reduced sensitivity of the mite's nervous system to the insecticide, allowing the mite to survive the treatment.
-Metabolic resistance: Increased levels of detoxifying enzymes in the mite, such as esterases, glutathione S-transferases, and cytochrome P450 monooxygenases, can enhance its ability to break down permethrin, reducing the overall insecticidal effect.
-Behavioral resistance: Mites may develop behavioral adaptations to avoid contact with the insecticide, such as changing their feedi
ng or resting patterns, thus reducing their exposure to the treatment.
Implications for Scabies Treatment
The emergence of permethrin-resistant scabies has significant implications for current treatment strategies. As resistance becomes more widespread, treatment failure rates may increase, leading to greater morbidity, prolonged outbreaks, and increased transmission rates. Consequently, there is an urgent need to develop new treatment options for scabies.
Several alternative treatments are currently under investigation, including ivermectin, benzyl benzoate, and moxidectin. Ivermectin, an oral medication, has shown promise as a potential alternative to permethrin. A 2019 Cochrane Review by Rosumeck et al. analyzed the efficacy of ivermectin compared to permethrin and other topical treatments for scabies.
https://pubmed.ncbi.nlm.nih.gov/31017622/
The review concluded that ivermectin was at least as effective as permethrin in treating scabies, with fewer side effects. However, more research is needed to establish the optimal dosing regimen and to assess the potential for ivermectin resistance.
Benzyl benzoate, a topical scabicidal agent, has also been considered as an alternative treatment option. While it has been used for scabies treatment for many years, it can cause skin irritation and is generally considered less effective than permethrin. Nonetheless, in the context of permethrin resistance, benzyl benzoate may still have a role to play in scabies management.
Moxidectin, an anthelmintic drug that has shown promise in treating other parasitic diseases, is currently being investigated for its potential use in scabies treatment.
A multicentre clinical phase II trial in humans is in progress in Australia and France, with the aim of developing moxidectin as a new single-dose treatment for scabies (NCT03905265).
Apart from pharmacological interventions, non-pharmacological strategies such as improved hygiene, environmental control measures, and community education can also help in managing scabies outbreaks and reducing the risk of resistance development.
Conclusion
The emergence of permethrin-resistant scabies is a growing concern for global public health. As scabies continues to evolve, so too must our approach to its treatment and management. Ongoing surveillance of resistance patterns, the development of alternative treatment options, and a focus on non-pharmacological strategies are critical to combating this persistent and highly contagious disease. By staying one step ahead of the ever-adapting scabies mite, the medical community can work towards a future where scabies no longer poses a significant threat to global health.
References:
https://www.sciencedirect.com/science/article/pii/S1198743X14614415
https://journals.asm.org/doi/10.1128/CMR.13.2.207
https://www.jaad.org/article/S0190-9622(83)80285-0/pdf
https://www.futuremedicine.com/doi/10.2217/17460913.3.1.57
https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0000354
https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0004389
https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0000444
For the latest on
Scabies, keep on logging to Thailand Medical News.