Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 17, 2024 1 year, 2 months, 19 hours, 19 minutes ago
COVID-19 News: Chronic pain is a pervasive and debilitating condition affecting millions worldwide, characterized by persistent discomfort lasting longer than three months and often accompanied by emotional distress and functional impairment. Musculoskeletal pain, originating from bones, joints, muscles, or related soft tissues, and neuropathic pain, arising from lesions or diseases of the somatosensory nervous system, constitute significant components of the chronic pain burden. However, the emergence of the COVID-19 pandemic has added a new layer of complexity to this already challenging landscape. Patients infected with COVID-19 have been reported to experience musculoskeletal and neuropathic pain either as a direct consequence of the virus or due to exacerbation of preexisting chronic pain conditions. In this comprehensive review covered in this
COVID-19 News report, conducted in collaboration between the University of Kansas Medical Center, Kansas City, USA, and the National Spine and Pain Centers, Frederick, MD, USA, the researchers aim to delve deeply into the epidemiology of pain pre-pandemic, the impact of COVID-19 on the body, mechanisms of pain, post-pandemic chronic pain management, and potential treatment options.
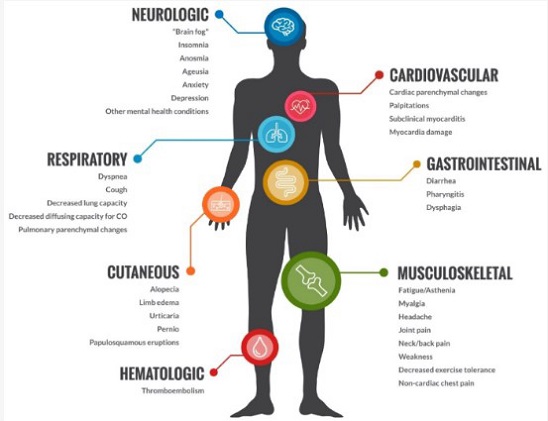
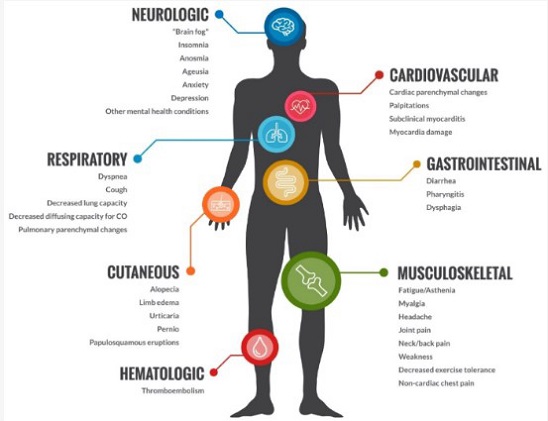 Effects of COVID on the body
Epidemiology of Musculoskeletal and Neuropathic Pain Pre-Pandemic
Effects of COVID on the body
Epidemiology of Musculoskeletal and Neuropathic Pain Pre-Pandemic
Before the onset of the COVID-19 pandemic, chronic pain posed a significant global health challenge, both in terms of individual suffering and healthcare costs. Musculoskeletal pain, including conditions such as low back pain, neck pain, and arthritis, accounted for a substantial portion of healthcare spending, with estimates reaching billions of dollars annually in the United States alone.
Epidemiological studies indicated a prevalence of musculoskeletal pain ranging from 13.5% to 47%, with risk factors including age, socioeconomic status, mental health, and occupational factors such as manual labor.
Similarly, neuropathic pain, characterized by abnormal sensations and neurologic deficits, affected a significant proportion of the population, with diverse etiologies ranging from diabetes and infections to trauma and cancer. The prevalence of neuropathic pain was estimated to be between 6.9% and 10.0%, although quantifying its exact burden remained challenging due to variability in assessment measures and subjective nature of reporting.
COVID-19 and Its Impact on Musculoskeletal and Neuropathic Pain
The COVID-19 pandemic has brought unprecedented challenges to individuals suffering from chronic pain. Beyond the acute respiratory symptoms commonly associated with COVID-19, growing evidence suggests a substantial impact on musculoskeletal and neuropathic pain. Patients infected with COVID-19 may experience post-viral musculoskeletal pain, with estimates suggesting a prevalence ranging from 5.65% to 18.15%. Long COVID, characterized by persistent symptoms following acute infection, further exacerbates this burden, with musculoskeletal manifestations such as fatigue, arthralgia, and myalgia being common.
Neuropathic pain has also emerge
d as a significant issue in the aftermath of COVID-19 infection, with proposed mechanisms including cytokine storms, neuroinflammation, and reactivation of dormant viruses. Patients may present with conditions such as post-herpetic neuralgia, trigeminal neuralgia, and brachial plexopathy, adding to the complexity of chronic pain management in the COVID-19 era.
Emerging Perspectives on Underlying Mechanisms in Chronic Pain in COVID-19
Understanding the pathophysiological mechanisms underlying chronic pain in the context of COVID-19 infection is essential for targeted treatment strategies. Several hypotheses have been proposed, including neuroinflammation, angiotensin-2 mediated effects, and sympathetic nervous system overactivity. Studies have shown a higher prevalence of new-onset chronic pain in COVID-19 patients, particularly those with risk factors such as higher BMI, older age, and underlying disorders.
Intensive care patients are particularly vulnerable, facing increased risks of myopathies, polyneuropathy, and muscle atrophy following COVID-19 infection. These complications contribute to persistent pain and pose challenges for healthcare providers in managing chronic pain in this population.
Management of Chronic Pain in the COVID-19 Era
The COVID-19 pandemic has necessitated a paradigm shift in the assessment and management of chronic pain patients. Telemedicine has emerged as a valuable tool, providing accessibility while minimizing exposure to the virus. However, challenges exist, particularly for patients with multiple comorbidities requiring in-person consultations and physical examinations.
The emotional impact of the pandemic on chronic pain patients cannot be overstated, highlighting the importance of comprehensive assessments considering both sensory and emotional components of pain. Multidisciplinary approaches to pain management, incorporating cognitive-behavioral therapy, guided meditation, exercise therapy, and pharmacologic interventions, have demonstrated efficacy in reducing chronic pain.
However, the closure of clinics and transition to telemedicine have disrupted traditional pain management approaches, leading to increased cancellations, delays, and reduced accessibility to services. Further research is needed to identify specific treatment strategies and develop evidence-based guidelines tailored to the unique needs of chronic pain patients in the COVID-19 era.
Novel Pharmacological Treatments
While no specific pharmacotherapy is currently FDA-approved for COVID-19-related chronic pain, various drug classes, including antihistamines and antidepressants, have been proposed as potential therapies. However, further research is needed to evaluate their efficacy and safety in this context.
Identification of pain phenotypes and precision pain guidelines for post-COVID-19 chronic pain remains an area of research. Treatment options for nociceptive pain, including NSAIDs, steroids, and physical therapy, have shown potential benefits, although caution is warranted due to cardiovascular and cerebrovascular risks associated with NSAID use.
Similarly, management of neuropathic pain in the context of COVID-19 remains challenging, with limited evidence supporting specific treatment approaches. Further research is needed to elucidate the underlying mechanisms and develop targeted interventions for this patient population.
Conclusion
In conclusion, the COVID-19 pandemic has significantly impacted individuals suffering from chronic pain, introducing new challenges and exacerbating existing ones. Understanding the mechanisms underlying COVID-19-related chronic pain is crucial for targeted interventions and improved patient outcomes. Multidisciplinary approaches to pain management, incorporating telemedicine, comprehensive assessments, and evolving models of care, are essential in mitigating the burden of chronic pain in the COVID-19 era. Further research is needed to identify specific treatment strategies and develop evidence-based guidelines tailored to the unique needs of chronic pain patients in this evolving healthcare landscape.
The study findings were published in the peer reviewed journal: Diagnostics.
https://www.mdpi.com/2075-4418/14/3/332
For the latest
COVID-19 News, keep on logging to Thailand Medical News.