Naïve T Cells Plays A Very Important Role As To Why Children With COVID-19 Have A Lower Mortality Risk!
Source: Naïve T Cells And SARS-CoV-2 Jan 15, 2022 3 years, 2 months, 4 weeks, 2 days, 20 hours, 47 minutes ago
Naïve T Cells And SARS-CoV-2: A new study by researchers from West China Hospital, Sichuan University, Chengdu-China has found that that naïve T cells plays a very important role as to why children with COVID-19 have a lower mortality risk.
A naïve T cell is a T cell that has matured and been released by the thymus but has not yet encountered its corresponding antigen. In other words, naïve T cells are in the stage between maturity and activation. Each naïve T cell has a unique T cell receptor (TCR) that recognizes a specific antigen.
Naïve T cells are precursors for effector and memory T cell subsets. Phenotypically, naïve T cells are small cells with little cytoplasm; they express surface markers, such as CD45RA, CCR7, CD62L, CD127, and CD132. They lack expression of markers of previous activation, such as CD25, CD44, CD69, CD45RO, or HLA-DR.
Naive T cells can respond to novel pathogens that the immune system has not yet encountered. Having adequate numbers of naive T cells is essential for the immune system to continuously respond to unfamiliar pathogens.
A peculiar phenomenon has been observed during the ongoing COVID-19 pandemic in that younger individuals especially children infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) had a lower mortality rate and fewer cases of death.
To date, it has always been assumed that the human immune system develops continuously from birth to adolescence, and that immunity to infections is strongest in early to middle adulthood, then begins to wane in late age.
So far, older COVID-19 patients, especially those over 70 years old, had a greater mortality rate than the others, as expected.
However, the severity of COVID-19 and its associated mortality is higher in young and middle-aged adults than in children, contrary to popular belief.
Because the immune system in early life (infancy and early childhood) is not fully developed, the severity of COVID-19 and its mortality should be higher in infants and children than in adults. However, this observation as not been observed in the current COVID-19 scenario.
Ironically, adults, who are expected to have superior immunity, have a higher mortality rate than small children, according to current data.
The
Naïve T Cells And SARS-CoV-2 study team from Sichuan University discuss how naïve T cells may contribute to lower mortality rates seen in children with COVID-19.
It is known that by expressing unique T-cell receptors (TCRs), naive T cells maintain their specificity while remaining uncommitted to their helper fate until they encounter antigens presented by antigen-presenting cells (APCs).
It has been found that every 12–24 hours, each naive T cell travels via the bloodstream to the lymph nodes, yet only 1 in 105 naive T cells respond to any specific antigen. If naive T cells do not bind to any of the major histocompatibility complex (MHC)/antigen complexes presented by the APC, they escape through the thoracic duct and return to the bloo
dstream. When a naive T cell comes into contact with the matching MHC/antigen complex, it becomes activated, proliferates, and differentiates into effector and memory T cells with antigen specificity that is similar.
Hence, the amount of naive T cells in the body could be crucial in supporting the body in detecting and dealing with SARS-CoV-2 infections.
The SARS-CoV-2 virus is a new pathogen that has never been met by anyone's immune system, young or old. As a result, there is no distinction between SARS-CoV-2 and common pediatric pathogens such as respiratory viruses, enteroviruses, and conditioned pathogenic bacteria in the immune systems of children. It is only necessary for the immune system to recognize it, activate adaptive immunity, and store memory T cells, which is similar to how these cells deal with other infections.
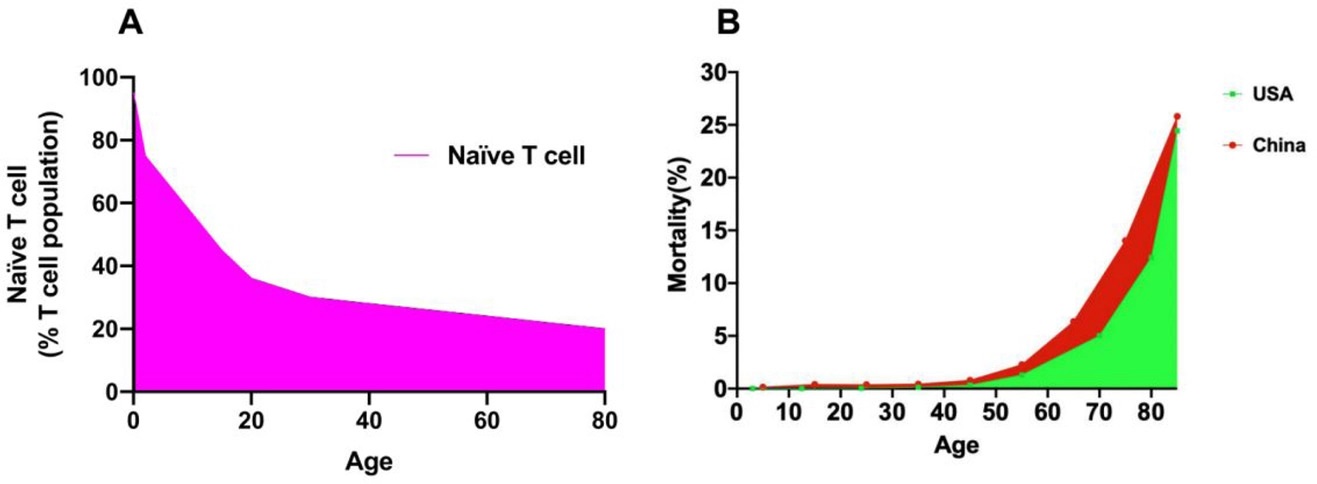 The naïve T-cell trend with increasing age is opposite to that of age-related mortality
The naïve T-cell trend with increasing age is opposite to that of age-related mortality
Importantly after childhood, however, the number of naive T cells decreases dramatically, and memory T cells become the dominant fraction throughout the body. As a result, the TCR diversity of naive T cells with the ability to recognize new antigens has been considerably reduced in adults, particularly in the elderly. It is possible that a T-cell clone expressing a specific TCR that can recognize SARS-CoV-2 cannot be picked after multiple rounds of naive T-cell patrol and circulation. Only innate immunity is triggered to remove pathogens if the immune system is unable to appropriately detect a novel antigen and activate the adaptive immune response, and the balance between viral proliferation and the innate immune response may be upset.
It should be noted that the fraction of naive T cells in COVID-19 patients is reported to be much lower, although the effector and memory subsets are correspondingly enhanced.
Typically, when the host is infected with a pathogen that has never been seen before, naive T cells are transformed into effector/memory T cells. Once a T-cell clone expressing a specific TCR that recognizes SARS-CoV-2 is found from the naive T-cell pool, that clone will differentiate into effector/memory T cells, resulting in a decrease in naive T cells and a rise in effector/memory T cells.
Importantly SARS-CoV-2-specific T cells were discovered in persons who had recovered from asymptomatic COVID-19 infections, which is reassuring.
SARS-CoV-2 infections have a substantially lower severity and fatality rate in children than it does in adults. The quantity of age-related naive T cells was not linearly associated with COVID-19 patient mortality, which could be owing to changes in TCR diversity and nave T cell survival.
Despite these changes may not be directly reflected in the number of naive T cells, they will have a major impact on the ability to identify new antigens.
Hence, rather than an "immune overreaction problem," the immune system in patients with severe instances may have a "pathogen identification problem."
Importantly this could be a simple explanation for why COVID-19-positive children exhibit minimal symptoms and a low mortality rate. Increasing the number of naive T cells or the diversity of TCRs may be a feasible technique to improve the host's ability to "search for and eliminate" developing lethal infections that have never been seen by the immune system, according to this new perspective.
The study findings were published in the peer reviewed Journal of Evidence-Based Medicine.
https://onlinelibrary.wiley.com/doi/10.1111/jebm.12454
For more on
Naïve T Cells And SARS-CoV-2, keep on logging to Thailand Medical News.
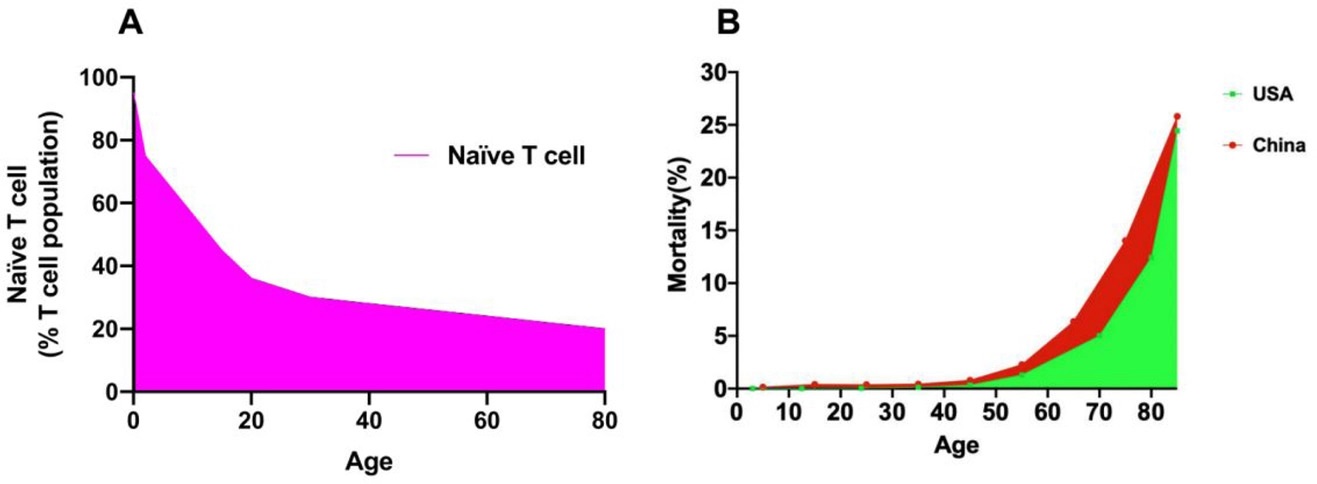 The naïve T-cell trend with increasing age is opposite to that of age-related mortality
The naïve T-cell trend with increasing age is opposite to that of age-related mortality