Navigating Vascular Complications of COVID-19: An Evolving Understanding and the Road Ahead
COVID-19 News - Vascular Complications of COVID-19 Apr 04, 2023 2 years, 2 weeks, 2 days, 12 hours, 50 minutes ago
The ongoing COVID-19 pandemic has posed numerous challenges to the global healthcare system. While respiratory symptoms have been the most prominent manifestation of the disease, an increasing number of vascular complications have been identified. A review published in the Canadian Journal of Cardiology, titled "An evolving understanding of the basis and management of vascular complications of COVID-19: Where do we go from here?" (2023), sheds light on these complications, our current understanding, and potential management strategies.
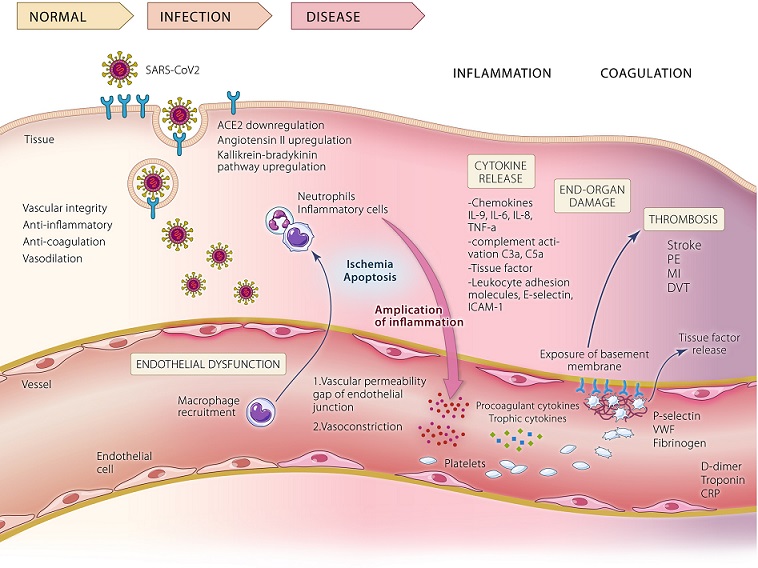
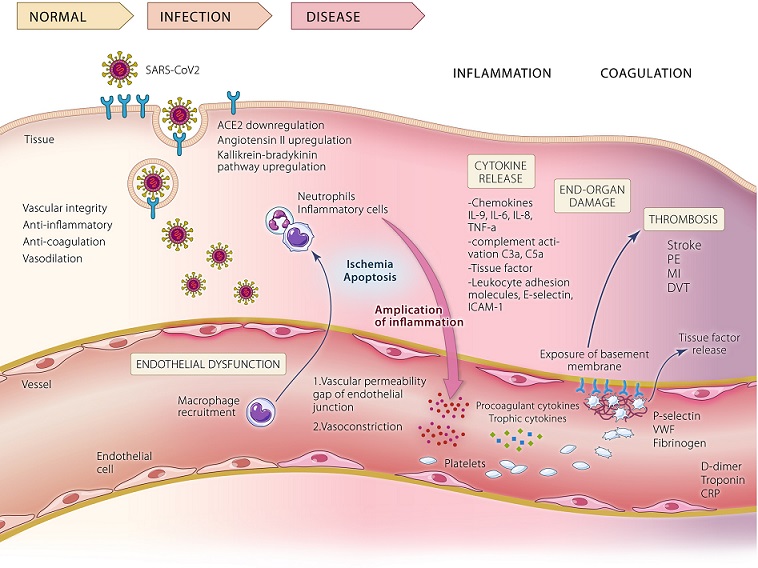 Pathophysiological mechanisms involved in COVID-19 vascular dysfunction and coagulopathy. During infection, SARS-CoV-2 gains entry to human cells via interaction of its spike protein with the angiotensin-converting enzyme 2 (ACE2) receptor. Downregulation of ACE2 activity, related accumulation of angiotensin-II and upregulation of the kallikrein-bradykinin pathway with a marked reduction in pericytes through apoptosis of infected cells contribute to the thrombo-inflammatory process. The diseased endothelium harms vascular integrity with consequent vascular leakage and vasoconstriction that induce ischemia and apoptosis. This leads to macrophage and complement activation, and further leucocyte recruitment. Amplification loops of the inflammatory response ensue, with overproduction of cytokines and immune mediators. At the time of endothelial injury and the consequent inflammatory response, exposure of a thrombogenic basement membrane can trigger coagulation pathways. Activation of the clotting cascade involves recruitment of platelets and release of trophic cytokines and procoagulant mediators, which are further enhanced by the expression of adhesion proteins (including P-selectin, von Willebrand factor and fibrinogen), increase in tissue factor activity, and suppression of fibrinolysis and thrombomodulin that ultimately results in thrombosis. Elevated inflammatory markers and hematological derangements such as thrombocytopenia and high levels of D-dimer and other fibrin breakdown products correlate with greater mortality risk and adverse outcomes.
Pathophysiological mechanisms involved in COVID-19 vascular dysfunction and coagulopathy. During infection, SARS-CoV-2 gains entry to human cells via interaction of its spike protein with the angiotensin-converting enzyme 2 (ACE2) receptor. Downregulation of ACE2 activity, related accumulation of angiotensin-II and upregulation of the kallikrein-bradykinin pathway with a marked reduction in pericytes through apoptosis of infected cells contribute to the thrombo-inflammatory process. The diseased endothelium harms vascular integrity with consequent vascular leakage and vasoconstriction that induce ischemia and apoptosis. This leads to macrophage and complement activation, and further leucocyte recruitment. Amplification loops of the inflammatory response ensue, with overproduction of cytokines and immune mediators. At the time of endothelial injury and the consequent inflammatory response, exposure of a thrombogenic basement membrane can trigger coagulation pathways. Activation of the clotting cascade involves recruitment of platelets and release of trophic cytokines and procoagulant mediators, which are further enhanced by the expression of adhesion proteins (including P-selectin, von Willebrand factor and fibrinogen), increase in tissue factor activity, and suppression of fibrinolysis and thrombomodulin that ultimately results in thrombosis. Elevated inflammatory markers and hematological derangements such as thrombocytopenia and high levels of D-dimer and other fibrin breakdown products correlate with greater mortality risk and adverse outcomes.
Vascular Complications of COVID-19
The review by researchers from Tel Aviv Sourasky Medical Center-Israel and University Health Network, Toronto-Canada highlights the growing evidence of vascular complications in COVID-19 patients. These complications include blood clot formation (thrombosis), inflammation of blood vessels (vasculitis), and damage to blood vessels (endothelial injury), which can lead to life-threatening events like strokes, heart attacks, and pulmonary embolism which have been covered in many studies and
COVID-19 News coverages. Factors such as older age, pre-existing medical conditions, and severe COVID-19 infection can increase the risk of vascular complications.
Understanding the Basis of Vascular Complications
The exact mechanisms underlying the vascular complications in COVID-19 are not fully understood, but several factors have been implicated:
-Hyperinflammation: The SARS-CoV-2 virus triggers an excessive immune response, leading to the release of inflammatory cytokines, which can damage blood vessels and promote clot formation.
-Endothelial dysfunction: The virus infects endothelial cells lining blood vesse
ls, causing direct injury and dysfunction. This increases the risk of clot formation and impairs blood flow regulation.
-Coagulation abnormalities: COVID-19 is associated with abnormalities in blood clotting factors, which can lead to increased clot formation and the risk of thrombotic events.
Management Strategies
The management of vascular complications in COVID-19 patients depends on early identification, risk stratification, and appropriate intervention. Some strategies highlighted in the study include:
-Anticoagulation therapy: Patients at high risk of clot formation may benefit from anticoagulant medications to prevent and treat thrombotic events.
-Anti-inflammatory treatment: Targeting the hyperinflammatory response with medications such as corticosteroids can help reduce the risk of vascular complications.
-Monitoring and follow-up: Close monitoring of patients at risk for vascular complications, with regular follow-ups and appropriate diagnostic tests, can help detect and manage these complications early.
Where Do We Go From Here?
Despite the advances in understanding the vascular complications of COVID-19, several questions remain unanswered. Future research should focus on:
-Identifying biomarkers: Developing accurate biomarkers to predict the risk of vascular complications can help guide early intervention and treatment strategies.
-Investigating novel therapies: Exploring new treatment options, including targeted therapies, to address the underlying mechanisms of vascular complications.
-Long-term implications: Assessing the long-term effects of COVID-19 on vascular health and the potential need for ongoing management in recovered patients.
Conclusion
The review provides valuable insights into the vascular complications of COVID-19 and highlights the need for continued research to better understand and manage these complications. By focusing on early identification, targeted treatment, and ongoing monitoring, healthcare professionals can help reduce the risk of life-threatening events in COVID-19 patients and improve patient outcomes.
The review was published in the peer reviewed Canadian Journal of Cardiology.
https://www.onlinecjc.ca/article/S0828-282X%2823%2900272-6/fulltext
For the latest
COVID-19 News, keep on logging to Thailand Medical News.