Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 14, 2024 5 months, 1 week, 5 days, 6 hours, 44 minutes ago
Medical News: Necrotizing pneumonia (NP) is a severe form of lung infection that, while rare, can turn deadly if not managed promptly. First identified in the 1940s, this aggressive pneumonia has been linked to mortality rates as high as 45% in severe cases. Unlike typical pneumonia, NP causes lung tissue destruction, leading to complications that often require specialized treatment. Despite its severity, there is limited research on how best to manage this condition, with most studies relying on retrospective reviews rather than clinical trials.
 Necrotizing Pneumonia- a Deadly Lung Infection
Necrotizing Pneumonia- a Deadly Lung Infection
This
Medical News report provides an updated comprehensive look into necrotizing pneumonia, explaining its causes, symptoms, and the latest treatment approaches. It serves as an informative guide for anyone interested in learning about this complex lung disease without delving too deeply into medical jargon.
What Is Necrotizing Pneumonia?
Necrotizing pneumonia results from a severe lung infection that damages lung tissues. In NP, the infection becomes so intense that it can create pockets of dead tissue, often leading to "holes" or cavities in the lungs. This damage typically stems from bacteria that infect the lung's blood vessels, blocking oxygen-rich blood from reaching certain areas and creating an environment conducive to tissue death.
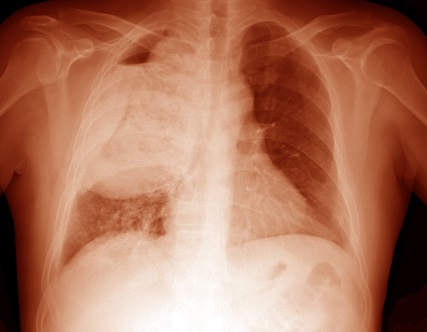
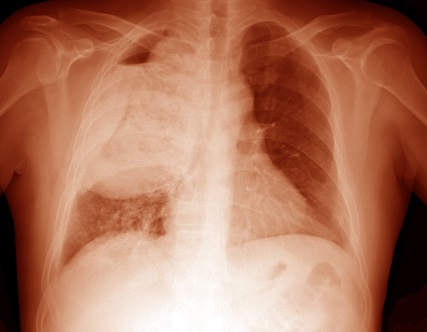
Diagnosing Necrotizing Pneumonia typically requires imaging such as CT scans, as regular chest X-rays may not always reveal the extent of damage. Unlike typical lung abscesses, which affect isolated areas, NP often appears in multiple lobes of the lungs. Necrotizing pneumonia can also cause septic pulmonary emboli - infected blood clots that travel from other parts of the body to the lungs, worsening the infection.
Epidemiology: How Common Is Necrotizing Pneumonia?
Necrotizing pneumonia is relatively uncommon, accounting for only around 1% of bacterial pneumonia cases. However, studies have shown it may often go undetected due to limited use of advanced imaging techniques. For instance, a 2024 study from the University of Louisville found that re-examining chest scans led to a higher diagnosis rate than initially reported. Other research has estimated that about 6.6% to 12% of people with community-acquired pneumonia (CAP) may develop necrotizing changes, often missed in early diagnostics.
What Causes Necrotizing Pneumonia?
The primary culprits behind NP are bacterial pathogens, including Streptococcus pneumoniae, Staphylococcus aureus, and Klebsiella pneumoniae. In children, other pathogens like Mycoplasma pneumoniae and Haemophilus influenzae are more commonly implicated. Interestingly, while some bacteria, such as Pseudomonas aeruginosa, rarely cause NP in healthy individuals, they can lead to severe cases in people with weakened immune systems.
Pathogenesis: How Does Necrotizing Pneumonia Develop?
Necrotizing pneumonia begins when bacteria enter the lungs, often through micro-aspiration or inhalation of i
nfected particles. This triggers an intense immune response in the airways, attracting immune cells to fight the infection. Unfortunately, this immune response can cause additional damage, particularly when certain bacterial toxins are involved. A notorious example is the Panton-Valentine leukocidin (PVL) toxin produced by some strains of Staphylococcus aureus, which damages white blood cells and worsens lung tissue necrosis.
A 2023 study showed that PVL-producing strains are 15 times more likely to cause NP than other strains. Similarly, S. pneumoniae serotype 3, which is not covered by current vaccines, is more likely to lead to necrotizing pneumonia because it can evade immune cells, allowing bacteria to proliferate and spread.
Who Is at Risk of Necrotizing Pneumonia?
Certain factors increase the risk of developing NP, including other infections like influenza and COVID-19, which can impair immune cell function and weaken the lungs. People with weakened immune systems, such as those undergoing chemotherapy, are also at a higher risk. Furthermore, lifestyle factors, including smoking, alcohol abuse, liver disease, and diabetes, increase susceptibility to NP. It’s also more prevalent in those with conditions like chronic obstructive pulmonary disease (COPD) and chronic kidney disease (CKD).
Signs and Symptoms of Necrotizing Pneumonia
Patients with necrotizing pneumonia typically experience rapid symptom onset, including fever, chest pain, cough, and shortness of breath. These symptoms resemble those of severe respiratory infections but tend to escalate quickly, often leading to sepsis - a dangerous body-wide response to infection. Complications like fluid buildup around the lungs (empyema) and severe coughing up blood (hemoptysis) are more common in NP than in other forms of pneumonia.
How Is Necrotizing Pneumonia Diagnosed?
Imaging techniques, especially CT scans, play a crucial role in diagnosing NP. This article explains that CT scans can show the extent of tissue necrosis and help distinguish NP from other lung conditions. In septic pulmonary emboli cases, CT scans reveal nodules and signs of lung tissue decay in over half of the patients.
Radiologists also look for "bulging fissures," which occur when the damaged lung tissue inflates and causes fissures in the lung to protrude outward, a unique sign of severe NP. Unfortunately, the differences between NP and other lung diseases, such as gangrene, often make diagnosis challenging, as these conditions overlap in their imaging characteristics.
Current Treatments for Necrotizing Pneumonia
Treating necrotizing pneumonia can be complex, involving a combination of antibiotics, supportive care, and sometimes surgery. Treatment typically starts with broad-spectrum antibiotics, with adjustments based on the identified bacteria. In hospital-acquired cases, treatment often includes additional MRSA-targeted antibiotics, such as linezolid or vancomycin, especially in patients with risk factors.
Empirical antibiotics are initially prescribed, especially if the patient has been hospitalized recently or has a history of infections. Recent guidelines suggest using antibiotics like linezolid, which suppresses toxin production, benefiting those with NP by reducing inflammation. However, short antibiotic courses, which are sometimes effective in regular pneumonia, usually do not work for NP due to the disease's severity and extensive tissue involvement.
The Role of Surgery in Treatment
Surgery remains a last-resort treatment for NP, typically reserved for patients who do not respond to antibiotics or have severe complications like bleeding. Surgical options include removing necrotic tissue or, in extreme cases, performing lobectomy (removal of an entire lung lobe). However, because of the high risks, many doctors prefer to avoid surgery when possible, opting instead for drainage procedures or non-surgical interventions.
Prognosis and Long-Term Outlook
Despite medical advances, NP remains a dangerous condition with a high mortality rate, especially in cases linked to PVL-producing S. aureus strains, where mortality can reach 56%. Several factors affect prognosis, including the need for mechanical ventilation, infection severity, and complications like airway bleeding. Studies have shown that NP patients require longer hospital stays than those with standard pneumonia, and they face a higher risk of long-term respiratory issues.
Future Directions for Necrotizing Pneumonia Research
Ongoing research aims to improve treatment protocols and patient outcomes for necrotizing pneumonia. Key areas of interest include understanding the optimal duration for antibiotic treatment and investigating potential benefits of adjuvant therapies like intravenous immunoglobulin (IVIG). There is also a growing interest in identifying biomarkers that could guide treatment decisions, allowing for a more tailored approach to managing this challenging disease.
Conclusion
Necrotizing pneumonia is an aggressive and potentially deadly form of lung infection. While rare, it can have devastating effects on patients’ lungs, often requiring long-term antibiotic therapy and, in severe cases, surgery. The unique pathogenesis of NP, often linked to toxin-producing bacteria, distinguishes it from other respiratory infections, and patients with underlying health conditions are at higher risk.
With improved diagnostic techniques and evolving treatment strategies, the hope is to improve patient outcomes and reduce mortality. However, due to the complexity of NP, it requires careful, individualized care.
The study review was published in the peer-reviewed journal: Pathogens.
https://www.mdpi.com/2076-0817/13/11/984
For the latest on Necrotizing Pneumonia, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/thailand-medical-study-finds-high-dose-of-sulbactam-with-colistin-lowers-mortality-in-deadly-pneumonia
https://www.thailandmedical.news/news/rapid-spread-of-new-super-strain-bacteria-threatens-asia