New COVID-19 Study Shows That SARS-CoV-2 S-Protein-Antibody Binding Strength And Hydrogen Bonds Quantity Are Temperature Dependent
Source: COVID-19 Study Dec 25, 2020 4 years, 4 months, 1 day, 13 hours, 47 minutes ago
A new
COVID-19 Study by scientist from McMaster University-Canada, Beijing Institute of Technology-China and Columbia University- USA has revealed that that SARS-CoV-2 spike and antibody binding strength and hydrogen bonds quantity are temperature dependent.
.jpg)
In their abstract, the study team said that the global efforts so far against the COVID-19 pandemic relies strongly on the human defense of antibody, which is assumed to bind the antigen’s Receptor Binding Domain with its Hypervariable Region(HVR).
Due to the similarity to other viruses such as SARS, however, the understanding of the antibody-virus interaction has been largely limited to the genomic sequencing, which poses serious challenges to the containment, vaccine exploration and rapid serum testing.
Based on the physical/chemical nature of the interaction, infrared spectroscopy was employed to reveal the binding disparity, when unusual temperature dependence was discovered from the 1550cm-1 absorption band, attributed to the hydrogen bonds by carboxyl/amino groups, binding the SARS-CoV-2 spike protein and closely resembled SARS-CoV-2 or SARS-CoV-1 antibodies.
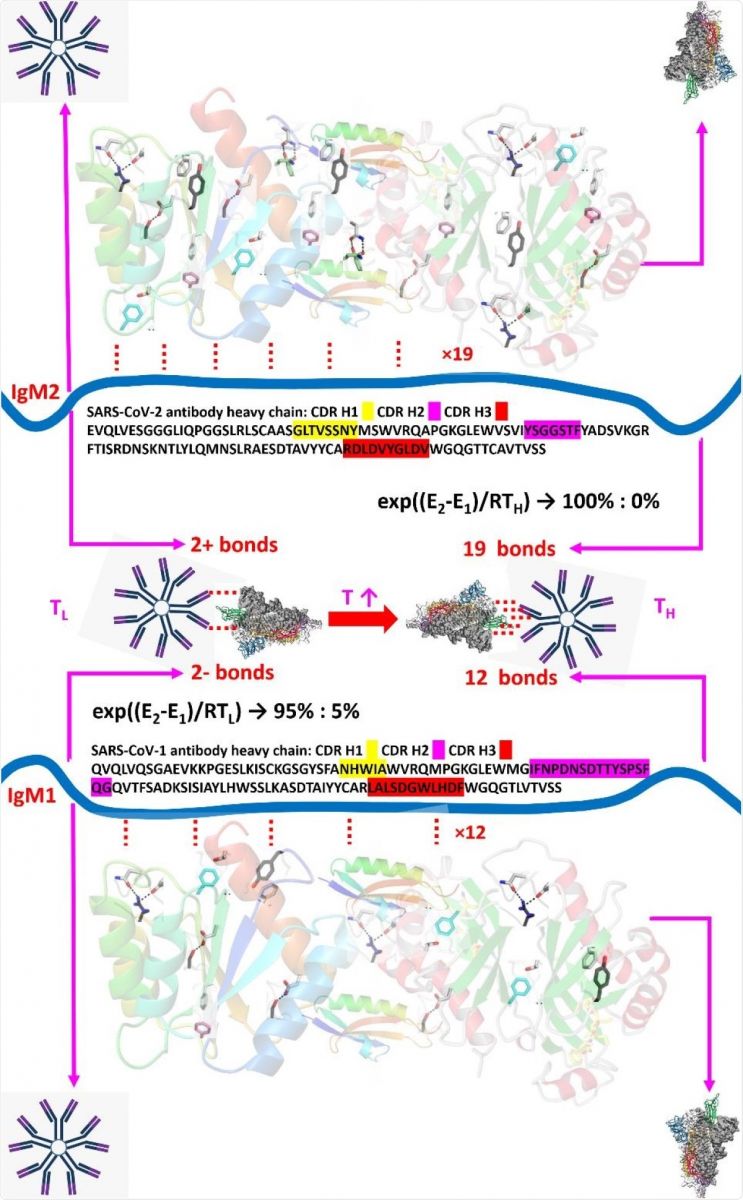
The infrared absorption intensity, associated with the number of hydrogen bonds, was found to increase sharply between 27°C and 31°C, with the relative absorbance matches at 37°C the hydrogen bonding numbers of the two antibody types (19 vs 12). Meanwhile the ratio of bonds at 27°C, calculated by thermodynamic exponentials rather than by the layman’s guess, produces at least 5% inaccuracy.
Hence as a result, the specificity of the SARS-CoV-2 antibody will be more conclusive beyond 31°C, instead of at the usual room temperature of 20°C - 25°C, when the vaccine research and antibody diagnosis would likely be undermined. Beyond genomic sequencing, the temperature dependence, as well as the bond number match at 37°C between relative absorbance and the hydrogen bonding numbers of the two antibody types, are not only of clinical significance in particular, but also of a sample for the physical/chemical understanding of the vaccine-antibody interactions in general.
The study findings were published on a preprint server and are currently being peer reviewed.
Numerous studies in this ongoing COVID-19 pandemic has focused on the role of neutralizing antibodies in countering infection by the SARS-CoV-2 coronavirus.
Most of these studies have been based on genome sequencing, showing matches between the Hypervariable Region (HVR) and the antigen’s receptor-binding domain (RBD). The results have been difficult to interpret, however, because of many factors, such as the rapid waning of antibody titers, as well as the shared antigenic sequences with many other viruses such as the earlier SARS (89% shared sequences) and influenza viruses.
Previous studies have addressed the similarity in the 3D structures of the spike protein in the two SARS viruses as seen on cryo-EM. When the amino acid sequences of the spike protein of the two viruses were compared, they showed a 77% similarity. Since this does not show the differences in binding, or the effect of temperature and other factors, or the nature of bonding, these studies have not been too successful.&
lt;br />
This research compared the binding strength of the SARS-CoV-2 and SARS-CoV spike protein-antibody complexes. Since it is thought that viral interactions with its angiotensin-converting enzyme 2 (ACE2) receptor or its IgM/IgG antibodies are via hydrogen bonding between carboxyl and amino groups, the investigators sought to use infrared spectroscopy (FTIR) to understand the nature of bonding as well as the number of bonds. This would help to estimate the intensity of viral attack.
Shockingly the study team found almost equal numbers of bonds for either virus at room temperature, or below 27°C. In other words, non-specific antibody reactivity was observed, with the accuracy being less than 95%. When the binding occurred at human body temperature, that is, at 37°C, or above 31°C, antibody specificity improved according to the number of available hydrogen bonds, at 19 and 12, respectively.
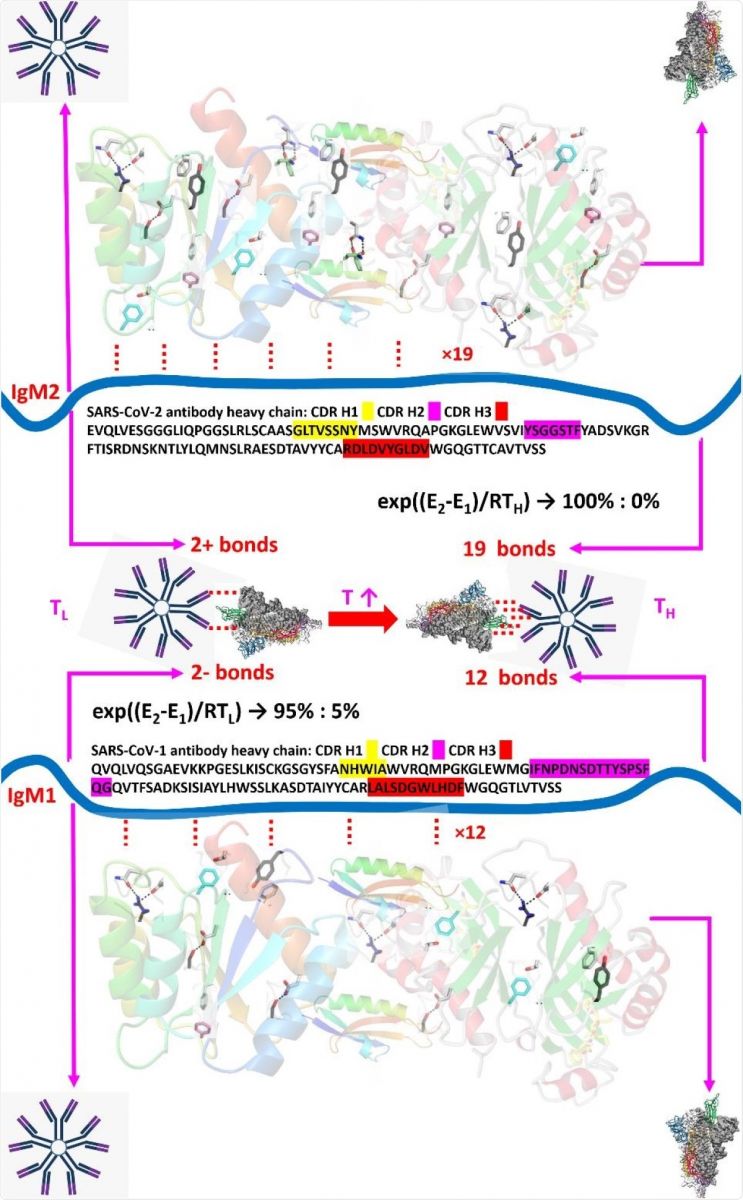 Analysis of antibody 2 and antibody 1 amino acid sequence with respect to the binding difference to the S protein. The IgM were depicted by the blue ribbon in the middle, and the S proteins represented by the screw ribbons in the top and bottom, where some of representative epitope residues in the S protein were labelled. Both antibodies form only 2+ hydrogen bonds at room temperature due to the folding of protein structure, while such number would increase to 19 and 12, respectively, at human body temperature. As can be calculated by the Arrhenius equation, around 5% of the S protein would bind with antibody 1 at room temperature, resulting in unavoidable testing inaccuracy which could only be eliminated at body temperature.
Analysis of antibody 2 and antibody 1 amino acid sequence with respect to the binding difference to the S protein. The IgM were depicted by the blue ribbon in the middle, and the S proteins represented by the screw ribbons in the top and bottom, where some of representative epitope residues in the S protein were labelled. Both antibodies form only 2+ hydrogen bonds at room temperature due to the folding of protein structure, while such number would increase to 19 and 12, respectively, at human body temperature. As can be calculated by the Arrhenius equation, around 5% of the S protein would bind with antibody 1 at room temperature, resulting in unavoidable testing inaccuracy which could only be eliminated at body temperature.
Possibly this was because of the further unfolding of the quaternary structure of the protein at higher temperatures.
It is known that thermal agitation leads to the thermal fracture of the van der Waals bonds between the protein strands, which reduce the number of such bonds. This led to the slow exposure of more hydrogen bonding sites.
Infrared spectroscopy or FTIR showed a similar absorbance at 1550 cm-1 for both mixtures, of the SARS-CoV-2 spike protein/SARS-CoV-2 antibody and the SARS-CoV-2 112 spike protein/ SARS-CoV-1 antibody, at 0.5% and 0.4%, respectively. In other words, the bonds between the antibodies and the spike proteins did not become stronger, but rather, a greater number of bonds were formed at higher temperatures.
This accounts for the higher specificity, since the higher ratio of bonds leads to an effective blockade of binding for non-specific antibodies.
The study findings results agree with recently published research that confirms the number of hydrogen bonds in both these virus-antibody complexes by amino acid sequencing and by comparing the heavy chains of the antibody molecules targeting both viruses.
Even with the close phylogenetic relationship and highly similar sequences found in SARS-CoV and SARS-CoV-2, infrared spectroscopy demonstrated the presence of different numbers of hydrogen bonds between the respective spike and antibody molecules.
The study team found a temperature-dependent rise in binding strength, probably due to the unfolding of the protein quaternary structure. This was found to be due to an increase in binding sites, and hence in the number of hydrogen bonds between the carboxyl and amino ends of the different proteins.
The study findings were supported by the absorbance findings at 37°C, when the number of hydrogen bonds of the two types of antibody, to SARS-CoV-2 and SARS-CoV respectively, was found to be 19 vs 11. At 27°C, the bond ratio calculated by thermodynamic exponentials is about 20:1, accounting for the non-specificity of binding at the lower temperature. Such information will help to estimate the accuracy of the newer Covid-19 IgM/IgG rapid antibody tests, that are intended to help with faster and broader tracking of vaccine responses, and of research on the virus, in general.
The study findings undoubtedly calls for the necessity of simulating human body temperature in the future antibody diagnosis, especially during the search for the possible vaccines, as the binding uniqueness, or the specificity of SARS-CoV-2 IgM/IgG, could only be fully obtainable at a warmer temperature, rather than under the usual lab/room temperature of 20°C - 25°C, where most of the vaccine research is conducted.
For the latest
COVID-19 Studies, keep on logging to Thailand Medical News.
.jpg)