Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 15, 2024 1 year, 3 months, 1 week, 5 days, 16 hours, 59 minutes ago
Medical News: A recent study has shed new light on how our immune system, particularly a type of immune cell known as cytotoxic CD8+ T cells, responds to SARS-CoV-2, the virus responsible for COVID-19. Researchers from various top institutions, including the University of Science and Technology of China and the MD Anderson Cancer Center in USA, collaborated to investigate the complex molecular interactions that occur during a COVID-19 infection. This
Medical News report explores the study's findings and explains how these immune cells can help fight off the virus.
 New discoveries on how the immune system fights COVID-19
How CD8+ T Cells Fight Infections
New discoveries on how the immune system fights COVID-19
How CD8+ T Cells Fight Infections
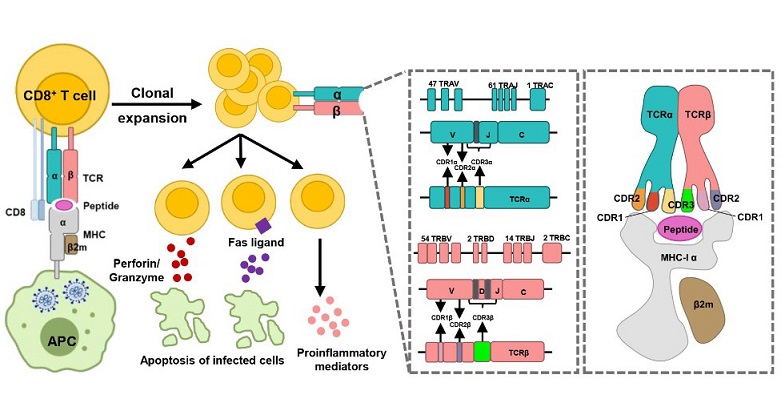
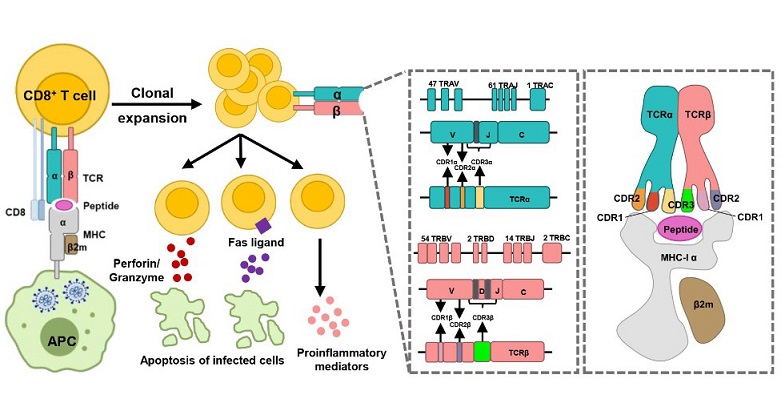
CD8+ T cells are a type of white blood cell that plays a key role in the immune response. They are often called "killer" T cells because they can directly kill infected cells. During a SARS-CoV-2 infection, these cells recognize infected cells and destroy them to stop the virus from spreading further in the body. The process begins when the immune system presents virus fragments, called antigens, on the surface of infected cells. CD8+ T cells recognize these antigens through a special receptor, known as T-cell receptors (TCR), which specifically binds to a combination of the antigen and a molecule called major histocompatibility complex (MHC).
The TCR-pMHC Interaction: The Key to the Immune Response
The interaction between T-cell receptors and the antigen-MHC complex is crucial for activating CD8+ T cells. When this interaction is successful, the CD8+ T cells are triggered to destroy the infected cells. However, not all individuals respond to the virus in the same way. Variations in the human leukocyte antigen (HLA) system, which is the part of the immune system responsible for presenting these virus fragments, can affect how well these interactions take place.
Researchers in this study found that certain HLA types are better at presenting SARS-CoV-2 antigens, leading to a stronger immune response. On the other hand, other HLA types are less efficient, which may explain why some people experience severe COVID-19 symptoms while others recover more easily. This difference in immune response is a key focus of the research.
How SARS-CoV-2 Escapes the Immune System
One of the most significant findings from this study is how SARS-CoV-2 can evade the immune system. The virus can mutate in ways that interfere with the presentation of its antigens on the surface of infected cells. This means that the CD8+ T cells are less able to recognize and attack the virus.
The study found that specific mutations in the virus disrupt the binding between the virus fragments and the MHC molecules, preventing proper recognition by the TCR. For example, certain mutations in the spike protein of the virus, which is a major target for both antibodies and T cells, were shown to reduce the effectiveness of CD8+ T cells in killing the virus.
Importance of TCR Diversity
T-cell receptors are incredibly diverse. Each person&
#39;s immune system has a unique set of TCRs that can recognize different virus fragments. The researchers highlighted the importance of this diversity in mounting an effective immune response. People with a broader range of TCRs are likely to have a better chance of recognizing and responding to new variants of SARS-CoV-2. However, as people age, the diversity of their TCRs tends to decrease, which may explain why older individuals are more vulnerable to severe COVID-19.
The study also pointed out that vaccination can help boost TCR diversity. Vaccines, particularly mRNA vaccines like Pfizer-BioNTech and Moderna, have been shown to stimulate a wide range of TCRs that recognize various parts of the SARS-CoV-2 virus. This suggests that vaccination not only helps in producing antibodies but also enhances the body’s ability to mount a strong T-cell response.
The Role of Memory T Cells
Another key finding of the study is the role of memory T cells. These are T cells that remain in the body after an infection or vaccination and can respond more quickly if the person is exposed to the virus again. The researchers found that SARS-CoV-2-specific memory T cells can persist for up to six months after infection or vaccination, providing long-term protection. This helps explain why some people who have recovered from COVID-19 or have been vaccinated continue to be protected even if their antibody levels decrease over time.
How This Study Helps in Vaccine Development
One of the major goals of this research is to help guide the development of future vaccines and treatments. By understanding which parts of the virus are most likely to trigger a strong T-cell response, scientists can design vaccines that better target those areas. This could lead to vaccines that provide longer-lasting immunity or that are more effective against new variants of the virus.
The study’s findings suggest that focusing on the parts of the virus that are less likely to mutate, or that are essential for the virus’s survival, could help in developing vaccines that remain effective as the virus evolves.
Conclusion
In conclusion, this study provides valuable insights into how the immune system responds to SARS-CoV-2 and why some people experience more severe symptoms than others. The role of CD8+ T cells, the importance of TCR diversity, and the ability of the virus to escape immune detection are all crucial factors in understanding and controlling the COVID-19 pandemic.
The researchers have opened new avenues for future research and vaccine development. Their findings underscore the importance of boosting both antibody and T-cell responses through vaccination and highlight the need for ongoing surveillance of viral mutations.
The study findings were published in the peer-reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1468456/full
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/cd81-fusion-protein-enhances-sars-cov-2-spike-trafficking-and-immune-response
https://www.thailandmedical.news/news/breaking-medical-news-study-discovers-that-memory-cd8-t-cells-causes-atherosclerosis-in-the-aged-by-promoting-plaque-buildup-of-the-arteries