Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 11, 2024 5 months, 5 days, 19 hours, 54 minutes ago
Medical News:
Researchers Identify Significant Reduction in Premature Ventricular Contractions After GI Treatments
In a groundbreaking study, researchers from the Sathyamoorthy Lab, Department of Medicine at Burnett School of Medicine-USA, Texas Christian University (TCU)-USA, have uncovered a fascinating link between premature ventricular contractions (PVCs) - a common type of heart arrhythmia - and upper gastrointestinal (GI) disorders. The research team, led by Dr Mohanakrishnan Sathyamoorthy and including a host of contributing experts, has shown that patients with a high burden of PVCs saw significant reductions in their symptoms following procedures to treat GI conditions.
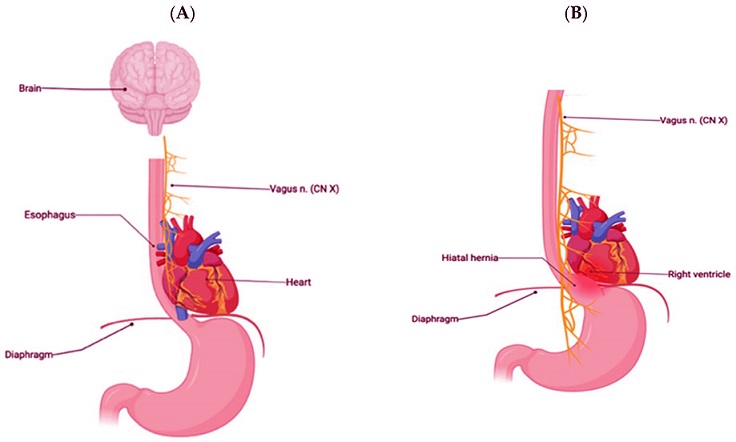
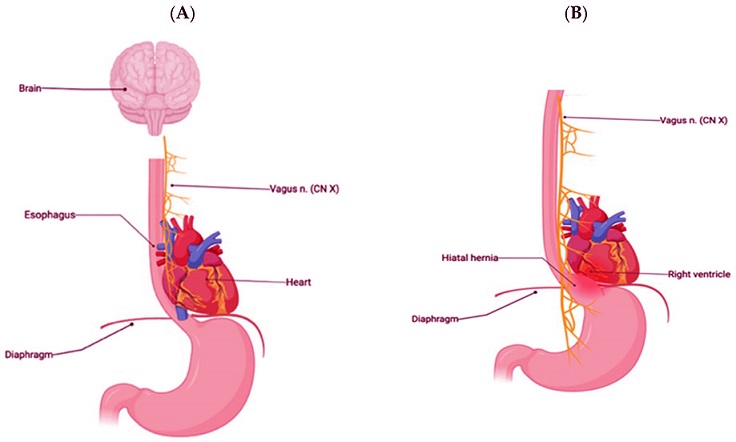 (A). Normal anatomic relationships of diaphragm, esophagus, vagus nerve, and heart. Note the very close anatomical proximity of the anterior esophagus to the vagus nerve to the posterior aspect of the right heart, in particular, the posterior aspect of the right ventricular outflow tract. (B). A hiatal hernia compressing the vagal nerve along with closer proximity to the right ventricle and posterior aspect of the RVOT in this altered anatomical state
PVCs and Their Potential Causes
(A). Normal anatomic relationships of diaphragm, esophagus, vagus nerve, and heart. Note the very close anatomical proximity of the anterior esophagus to the vagus nerve to the posterior aspect of the right heart, in particular, the posterior aspect of the right ventricular outflow tract. (B). A hiatal hernia compressing the vagal nerve along with closer proximity to the right ventricle and posterior aspect of the RVOT in this altered anatomical state
PVCs and Their Potential Causes
Premature ventricular contractions are extra heartbeats that disrupt the heart’s regular rhythm. They often originate from the right ventricular outflow tract (RVOT), which is near the esophagus. For years, these arrhythmias were thought to be benign; however, recent studies have suggested links between frequent PVCs and more serious cardiovascular issues.
The present study found a unique association suggesting that upper GI issues may trigger PVCs, with symptoms improving significantly after GI interventions. This
Medical News report explores how PVCs could potentially be caused by disruptions in the upper GI tract and highlights the notable improvements in patients after GI procedures.
Exploring the Vagus Nerve Connection
The researchers suggest that the vagus nerve, which serves both the heart and GI tract, may be the link between the heart arrhythmias and GI conditions. The vagus nerve runs along the esophagus and interacts with the heart, potentially triggering PVCs if disrupted by nearby GI issues.
This nerve connection could mean that certain GI diseases like gastroesophageal reflux disease (GERD), hiatal hernias, or esophageal dilation affect the heart by causing pressure on the vagus nerve. Some patients in the study experienced “vagally mediated” PVCs, indicating a dual mechanism of vagal stimulation and direct physical effects of GI disease on heart rhythms.
Detailed Study Findings and Results
In the study, six patients who had been diagnosed with upper GI disorders and high PVC burden underwent GI procedures such as hernia repairs and esophageal dilations. All patients demonstrated a high percentage of PVCs, originating from the RVOT, prior to their procedures.
After their respective interventions, researchers observed an impressive average reduction in
PVC burden of 68.34%, with most patients experiencing symptom relief. This reduction, verified by Holter monitoring, indicated that treating the GI conditions was effective in reducing PVCs, providing evidence of the connection between the two. For instance, a patient with a hiatal hernia showed nearly complete elimination of PVCs following hernia repair surgery.
Case Studies: Individual Success Stories
The study presents specific cases, each revealing the significant changes in PVC burden after GI interventions. One patient, a 60-year-old woman with severe GERD, underwent a LINX procedure to address her hiatal hernia. Prior to surgery, she exhibited PVCs in over 26% of her heartbeats. Post-surgery, her PVCs dropped to less than 1%, demonstrating how GI interventions can provide meaningful relief from heart arrhythmias.
Another patient, a 74-year-old man with esophageal stenosis, experienced similar improvements after undergoing esophageal dilation. His PVC burden decreased from 12.3% to 7.7%, showcasing that addressing the esophageal condition helped alleviate his arrhythmia symptoms.
How the Upper GI Tract and Heart Interact
Understanding why PVCs occur near the RVOT has long puzzled researchers, but the TCU team’s findings suggest that physical proximity and nerve connections play a major role. The esophagus, vagus nerve, and right ventricle are closely positioned, meaning any expansion or abnormality in the esophagus can press on the heart or irritate the vagus nerve, leading to arrhythmias.
One theory is that GI issues increase esophageal size, especially after meals. When the esophagus expands, it may compress the vagus nerve or place direct pressure on the RVOT, triggering PVCs. As a result, procedures that reduce esophageal swelling or tension could relieve these arrhythmias.
Supporting Evidence from Previous Studies
This finding aligns with previous research indicating that GI diseases can influence cardiac conditions. In particular, conditions like hiatal hernia and GERD have been linked with cardiac events, possibly due to inflammation or irritation from acid reflux. In one previous case, a patient experienced complete relief from atrial fibrillation (AF) after a hiatal hernia repair, leading researchers to speculate about vagus nerve involvement in arrhythmia cases related to the upper GI tract.
For years, swallow syncope, or fainting triggered by swallowing, has illustrated the vagus nerve’s effect on heart function. Swallowing can stimulate the vagus nerve, sometimes leading to sudden drops in blood pressure and heart rate. While rare, swallow syncope highlights how interconnected the heart and esophagus are, and why GI disorders may lead to abnormal heart rhythms like PVCs.
Next Steps for Research and Treatment
While the study’s findings are groundbreaking, the researchers acknowledge that further studies with larger sample sizes are needed to confirm the observed connection. This research could lead to new diagnostic protocols for arrhythmias, where doctors consider underlying GI conditions in patients with unexplained PVCs.
In the future, larger studies could establish GI treatments as a first-line defense against PVCs. The team believes this new understanding might lead to the classification of “E-PVCs,” or esophageal-PVCs, which could help patients receive more effective treatments tailored to their unique physiological conditions.
Conclusion: Expanding the Horizons of Heart-Related GI Treatments
This study highlights a potential shift in our understanding of arrhythmias. The reduction in PVC burden in all six patients after upper GI interventions emphasizes the close relationship between the GI tract and cardiac function. This revelation could lead to more holistic approaches for managing PVCs, especially in patients with high PVC burdens who also have GI conditions.
These findings open doors for further exploration into treating arrhythmias by addressing seemingly unrelated GI issues. If larger studies confirm these results, patients could benefit from a new subset of arrhythmia treatments focused on their GI health.
For patients and doctors alike, this study is a reminder of how interconnected our body systems are. Understanding these links will lead to more comprehensive, effective treatments for arrhythmias and other cardiac issues.
The study findings were published in the peer-reviewed journal: Hearts.
https://www.mdpi.com/2673-3846/5/4/38
For the latest on Arrhythmias, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/new-insights-from-stem-cell-research-reveals-role-of-inflammation-and-macrophages-in-atrial-fibrillation
https://www.thailandmedical.news/news/chinese-scientists-uncover-how-covid-19-triggers-arrhythmia