Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 22, 2024 1 year, 1 month, 3 weeks, 1 day, 6 hours, 54 minutes ago
Medical News: A recent study by a team of researchers from Griffith University in Australia may bring new treatment possibilities for people suffering from virus-induced osteoarthritis. Joint inflammation and pain, long known to accompany various viral infections like SARS-CoV-2, are often underexplored. However, researchers have now uncovered a key mechanism linking viral infections to joint damage, unlocking a potential therapy. The study shows how the viral spike protein in SARS-CoV-2 interacts with the body’s endothelin-1 (ET-1) signaling pathway, leading to osteochondral damage. This could pave the way for new treatments that target these pathways to alleviate joint damage and inflammation.
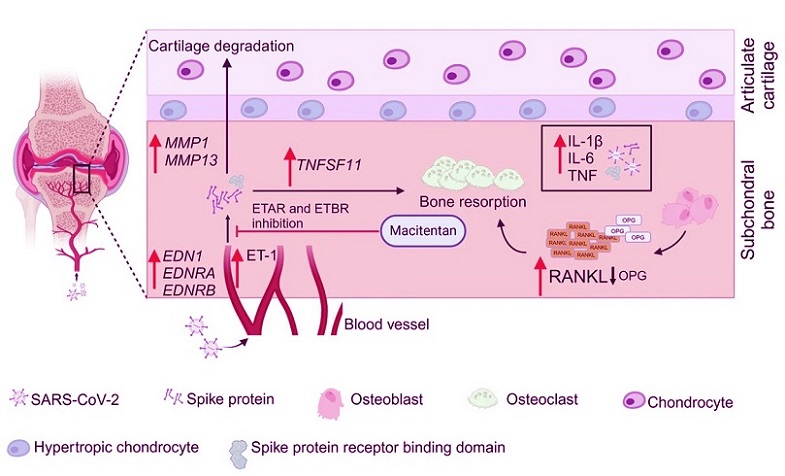
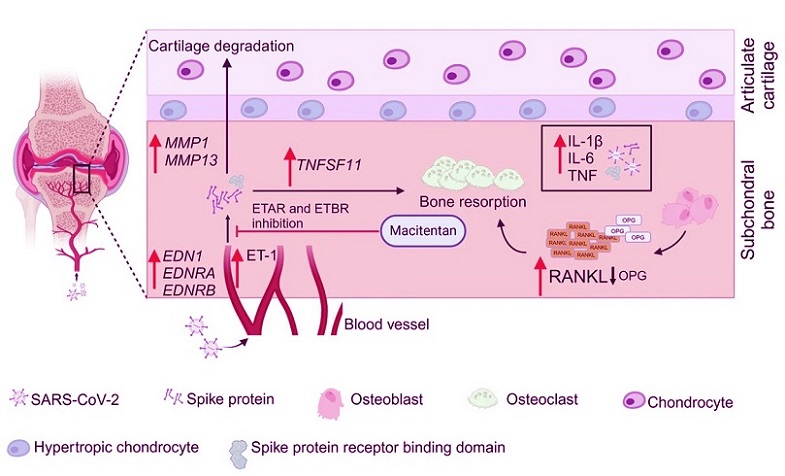 Proposed model for the development of SARS-CoV-2 induced osteoarthritis.
Proposed model for the development of SARS-CoV-2 induced osteoarthritis.
SARS-CoV-2 infection induces osteochondral damage by activating the interaction between the viral spike protein and the ET-1 signaling pathway. ET-1 increases vascular permeability, facilitating the infiltration of inflammatory cells into joint tissues and elevating levels of TNF, IL-6, and IL-1β. The spike protein activates RANKL, disrupting the RANKL-OPG balance, while also upregulating MMP1 and MMP13, leading to collagen breakdown, bone resorption, and cartilage degradation. The effect of ET-1 can be mitigated by using Macitentan, which helps alleviate SARS-CoV-2-induced joint damage.
The research, led by Dr. Wern Hann Ng, Patrick Chun Hean Tang, and Suresh Mahalingam from the Institute for Biomedicine and Glycomics at Griffith University-Australia, highlights that targeting the ET-1 signaling pathway using macitentan, a drug already approved for pulmonary arterial hypertension, could mitigate the joint damage caused by viral infections, particularly SARS-CoV-2. This
Medical News report explores their findings and what this means for people suffering from post-viral osteoarthritis.
Viruses and Osteoarthritis
It is well known that several viruses can lead to musculoskeletal issues, including joint pain, inflammation, and in some cases, osteoarthritis (OA). Viruses like the human immunodeficiency virus (HIV), hepatitis viruses, Epstein-Barr virus, and chikungunya have all been associated with joint diseases. These viruses often cause inflammation in the joints and muscles, leading to conditions like arthritis.
The most recent concern in this regard has been SARS-CoV-2, the virus behind COVID-19. Numerous patients have reported musculoskeletal pain and joint inflammation following infection. However, until now, the mechanisms behind these viral-induced conditions were not fully understood.
In this study, the research team delved into how the spike protein of SARS-CoV-2 interacts with the ET-1 signaling pathway. The study sheds light on the process and highlights the therapeutic potential of macitentan, an ET-1 receptor antagonist.
The Role of Endothelin-1 in Joint Damage
Endothelin-1 (ET-1) is a powerful vasoconstrictor known for its role in regulating vascular tone and blood flow. In recent years, ET-1 has been increasingly recognized for its involvement in inflammat
ory processes and tissue damage. Researchers in this study found that the SARS-CoV-2 spike protein elevated levels of ET-1 in infected individuals. This elevation in ET-1 levels contributed to increased vascular permeability, allowing inflammatory cells to infiltrate joint tissues.
Moreover, the researchers discovered that the viral spike protein also triggered an imbalance in bone remodeling processes. Specifically, it disrupted the balance between RANKL (Receptor Activator of Nuclear Factor Kappa-Β Ligand) and OPG (osteoprotegerin), which are critical in bone formation and resorption. This imbalance promoted bone resorption, leading to joint damage.
Additionally, the spike protein increased the expression of matrix metalloproteinases (MMP1 and MMP13), enzymes responsible for breaking down collagen in cartilage. These actions collectively contribute to the bone loss and cartilage degradation seen in osteoarthritis.
Macitentan: A Potential Treatment
In their experiments, the researchers used macitentan, a drug already approved by the FDA for treating pulmonary arterial hypertension. This drug works by blocking ET-1 receptors, effectively inhibiting the actions of ET-1. In a hamster model of SARS-CoV-2 infection, the researchers found that macitentan reduced joint damage, inflammation, and bone resorption.
More specifically, macitentan decreased vascular permeability, lowered inflammatory cytokine production, and inhibited MMP activation. These effects helped preserve joint cartilage and bone structure in the infected hamsters, providing hope that the drug could be repurposed to treat virus-induced osteoarthritis in humans.
Link to Human Cases
One of the most significant questions arising from the study is whether the findings in hamsters are applicable to human cases. The researchers examined computed tomography (CT) scans of two COVID-19 patients and found joint deterioration months after their infections. These patients displayed signs of osteoarthritis, such as cystic formations and narrowing of joint spaces. However, direct measurements of ET-1 or other related factors were not conducted in these patients.
Despite this limitation, the study found parallels between the hamster model and clinical observations in COVID-19 patients. For example, other studies have reported elevated levels of ET-1 in COVID-19 patients. Additionally, the altered RANKL/OPG ratios and reduced OPG levels observed in hamsters have also been noted in COVID-19 patients. This suggests that the mechanism identified in the hamster model might extend to humans as well.
Further Experiments on Human Cells
To bridge the gap between the animal model and human applications, the researchers conducted experiments on human endothelial cells (HUVEC) and mesenchymal stem cell-differentiated chondrocytes. The results showed that ET-1 significantly disrupted the balance of RANKL and OPG in human cells, mimicking the findings in the hamster model. Furthermore, in chondrocytes, a combination of spike protein, ET-1, and a neutralizing antibody led to increased cellular senescence markers, further linking the SARS-CoV-2 spike protein to long-term joint damage.
These findings provide strong evidence that macitentan could be used to treat COVID-19-induced osteoarthritis in human patients, although further research is needed to confirm these effects in clinical trials.
Conclusions
This study has opened the door to new treatment possibilities for people suffering from virus-induced osteoarthritis, particularly those dealing with post-COVID-19 joint damage. The researchers’ discovery of the link between the viral spike protein of SARS-CoV-2 and the ET-1 signaling pathway represents a significant step forward in understanding the mechanisms of viral-induced joint damage. By targeting ET-1, it may be possible to reduce joint inflammation, prevent bone resorption, and preserve cartilage in affected individuals.
The use of macitentan, a drug already approved for other conditions, is particularly promising. Its ability to block ET-1 receptors and mitigate joint damage in the hamster model suggests that it could be repurposed for treating post-viral osteoarthritis in humans. However, as with all animal studies, caution must be exercised when translating these findings to human patients. Clinical trials will be essential in determining the safety and effectiveness of macitentan for treating post-viral osteoarthritis, particularly in long-COVID cases.
The study findings were published in the peer-reviewed journal: NPJ (Viruses) by Nature.
https://www.nature.com/articles/s44298-024-00064-y
For the latest on Osteoarthritis, keep on logging on to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/cinnamaldehyde-treated-exosomes-shows-promise-in-treating-joint-inflammation
https://www.thailandmedical.news/news/melatonin-a-potential-game-changer-in-arthritis-treatment