New insights into mitochondrial role in post-COVID recovery and long COVID progression
Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 17, 2024 7 months, 1 week, 2 days, 11 hours, 41 minutes ago
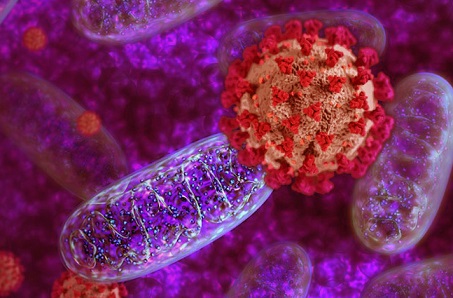
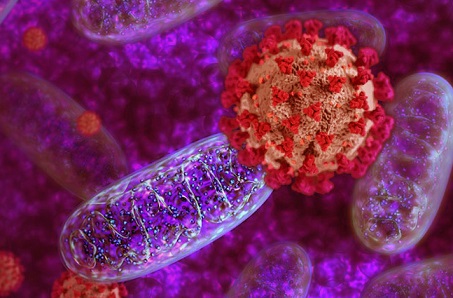
Medical News: As the world continues to grapple with the long-term consequences of the COVID-19 pandemic, researchers are increasingly turning their attention to long COVID - a condition marked by persistent symptoms long after the initial infection has subsided. New findings shed light on the pivotal role that mitochondrial function may play in recovery from COVID-19, as well as the development of long COVID. In this
Medical News report, we will explore these groundbreaking insights, focusing on how mitochondrial gene signatures could be essential to both recovery and the onset of long COVID.
 New insights into mitochondrial role in post-COVID recovery and long COVID progression
The Role of Mitochondria in COVID Recovery
New insights into mitochondrial role in post-COVID recovery and long COVID progression
The Role of Mitochondria in COVID Recovery
Mitochondria, known as the "powerhouses" of our cells, are central to producing the energy that our bodies need to function. However, they also play a key role in immune system responses and regulating inflammation, which are both critical in the body’s fight against infections like COVID-19. When functioning properly, mitochondria help the body repair itself and regulate immune activity. However, during infections such as COVID-19, mitochondrial function can become disrupted, potentially leading to prolonged symptoms, as seen in individuals with long COVID.
American researchers from the University of Southern California’s Leonard Davis School of Gerontology, the Keck School of Medicine, and the Feinberg School of Medicine at Northwestern University conducted studies to investigate the relationship between mitochondrial function and post-COVID outcomes. They aimed to understand how variations in mitochondrial gene expression may influence recovery from COVID-19, particularly in individuals who develop long COVID symptoms.
Mitochondrial Gene Signatures and Long COVID
The study examined blood samples from individuals who had recovered from COVID-19 and those who experienced long COVID, comparing them with samples from individuals who had never contracted the virus. The focus was on identifying changes in mitochondrial gene expression - specifically, genes that are involved in energy production and immune regulation. Results showed that individuals with long COVID had significantly different mitochondrial gene expression patterns compared to those who fully recovered.
In the early stages of post-COVID recovery (0-3 weeks after infection), those who later developed long COVID exhibited elevated mitochondrial activity, which may indicate a strong stress response within cells. This prolonged mitochondrial dysregulation was associated with a range of long COVID symptoms, including fatigue, brain fog, and persistent inflammation. In contrast, individuals who made a full recovery demonstrated more balanced mitochondrial gene activity, suggesting that early repair mechanisms were more successful in these patients.
Mitochondrial-Derived Peptides (MDPs): Key to Recovery?
One of the study’s key findings was the role of mitochondrial-derived pept
ides (MDPs) in regulating mitochondrial health. MDPs are small proteins produced by the mitochondria that help signal repair processes and reduce stress within cells. Three key MDPs - humanin, MOTS-c, and SHMOOSE - were analyzed in blood samples from both long COVID and recovered patients. In individuals who recovered fully, MDPs appeared to be more effective in regulating inflammation and promoting cellular repair.
Humanin and MOTS-c, in particular, were found to be negatively correlated with several markers of inflammation, indicating that these peptides may help mitigate the body’s inflammatory response during the early stages of COVID recovery. In contrast, individuals with long COVID showed positive correlations between these peptides and inflammatory biomarkers, suggesting that ongoing inflammation might overwhelm the protective effects of MDPs, contributing to the persistence of symptoms.
Inflammation and Mitochondrial Dysfunction in Long COVID
Another important aspect of the study was its focus on the relationship between inflammation and mitochondrial dysfunction. Persistent inflammation has been identified as a hallmark of long COVID, and the study’s findings suggest that mitochondrial dysfunction may be a key driver of this inflammatory response. In individuals with long COVID, the ongoing disruption of mitochondrial gene activity appeared to fuel inflammation, creating a vicious cycle that hindered recovery.
The study highlighted specific inflammatory biomarkers - such as TNF, IL-1B, and IL-18 - that were elevated in individuals with long COVID. These biomarkers are known to be associated with immune system overactivation and chronic inflammation, which are commonly observed in long COVID patients. Interestingly, these biomarkers also have direct links to mitochondrial dysfunction, further emphasizing the crucial role that mitochondria play in regulating the body’s response to COVID-19.
Long-Term Implications for Treatment
The findings from this study have significant implications for the treatment and management of long COVID. By identifying the role of mitochondrial dysfunction in the progression of long COVID, researchers may be able to develop targeted therapies that focus on improving mitochondrial health. This could include interventions aimed at reducing inflammation, enhancing mitochondrial repair processes, and boosting the activity of mitochondrial-derived peptides like humanin and MOTS-c.
Furthermore, these insights could help identify individuals at risk of developing long COVID early in their recovery, allowing for more proactive management of their symptoms. For example, monitoring mitochondrial gene activity and inflammatory biomarkers in the weeks following a COVID-19 infection could provide valuable information about a patient’s likelihood of experiencing prolonged symptoms.
Conclusion: Mitochondria as a Target for Long COVID Therapies
This study provides critical evidence that mitochondrial dysfunction plays a central role in the development of long COVID, while efficient mitochondrial repair mechanisms are essential for a full recovery. The persistent dysregulation of mitochondrial genes and elevated inflammatory responses in long COVID patients highlight the need for targeted therapies that focus on restoring mitochondrial health.
By better understanding the role of mitochondria in post-COVID recovery, researchers are paving the way for new treatments that could improve outcomes for millions of individuals worldwide who are still struggling with the effects of long COVID. The study’s findings emphasize the importance of early intervention and suggest that supporting mitochondrial function could be a promising avenue for preventing and managing long COVID.
The study findings were published on a preprint server and are currently being peer reviewed.
https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4950019
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/mitochondria-s-evolving-role-in-immunology
https://www.thailandmedical.news/news/covid-19-and-our-cells-powerhouses-mitochondria