Source: Society of Nuclear Medicine and Molecular Imaging Aug 08, 2018 6 years, 8 months, 2 weeks, 5 days, 23 hours, 56 minutes ago
Researchers have discovered a new nuclear medicine test that could improve care of patients with type 1 diabetes. The new positron emission tomography (PET) imaging method could measure beta-cell mass, which would greatly enhance the ability to monitor and guide diabetes therapies. This study is reported in the featured article of the month in
The Journal of Nuclear Medicine's August issue.
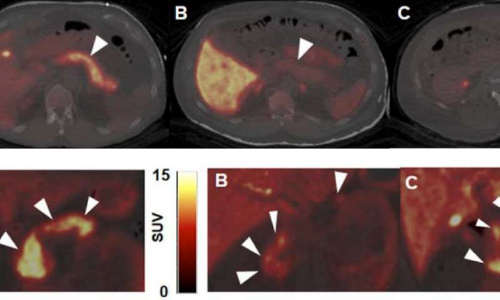
TOP: Representative axial slices of PET/CT overlay of pancreas uptake (white arrows) for each dopaminergic radioligand A) 11C-(+)-PHNO B) 11C-FLB457 and C) 11C-raclopride. All SUV images summed from 20-30 minutes. BOTTOM: Representative coronal PET/CT images of 11C-(+)-PHNO in pancreas (white arrows) for A) healthy control B) C-peptide deficient T1DM subject C) T1DM subject with detectable C-peptide All SUV images are summed from 20-30 minutes. Credit: J Bini et al., Yale University, New Haven, CT.
According to the American Diabetes Association, approximately 1.25 million American children and adults have type 1 diabetes. Jason Bini, Ph.D., at the Yale University PET Center in New Haven, Connecticut, explains the significance to patients of being able to track their beta-cell mass:
"Beta-cell mass includes both functional and non-functional beta cells. Many indirect methods to measure beta-cell function are influenced by factors such as glucose and insulin levels and are not able to measure non-functional (dormant) beta cells that may be responsive to treatments. This work is important for patients because uptake of a radiotracer measured on a PET scan could guide treatment options. For example, if a patient has low beta-cell function with high signal in the PET scan, this could represent a patient with dormant beta cells that could respond to a treatment targeting existing cells. If a patient has low beta-cell function and low signal in the PET scan (very few viable or dormant beta cells present), that individual may be a candidate for beta-cell transplantation."
Beta cells and neurological tissues have common cellular receptors and transporters, so, the Yale researchers screened brain radioligands for their ability to identify
beta cells. Then, 12 healthy control subjects and two subjects
with type 1 diabetes mellitus underwent dynamic PET/CT scans with six tracers.
The dopamine type 2/type 3 (D2/D3)-receptor agonist radioligand carbon-11 (
11C)-(+)-4-propyl-9-hydroxynaphthoxazine (PHNO) was the only radioligand to demonstrate sustained uptake in the pancreas with high contrast versus abdominal organs such as the kidneys, liver, and spleen.
The results provide preliminary evidence that
11C-(+)-PHNO is a potential marker of beta-cell mass with 2:1 binding of D3 receptors over D2 receptors. While further research is needed before clinical application,
11C-(+)-PHNO is a promising way to differentiate the beta-cell mass of healthy individuals from those with type 1 diabetes mellitus, as well as track and guide therapies for diabetes
patients.
Bini also points out, "These findings could facilitate development and wider dissemination of novel imaging methods in molecular imaging and
xpress.com/tags/nuclear+medicine/">nuclear medicine to assess receptor/enzyme pharmacology in
diabetes and other endocrine disorders."
Reference: Jason Bini et al, Evaluation of PET Brain Radioligands for Imaging Pancreatic β-Cell Mass: Potential Utility of11C-(+)-PHNO,
Journal of Nuclear Medicine (2018). DOI: 10.2967/jnumed.117.197285