New Strains Of Malaria Parasites With Mutations That Evade Diagnostics And Drugs Has Emerged In Ethiopia!
Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 22, 2024 1 year, 3 months, 4 days, 8 hours, 34 minutes ago
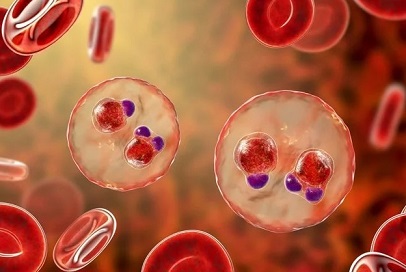
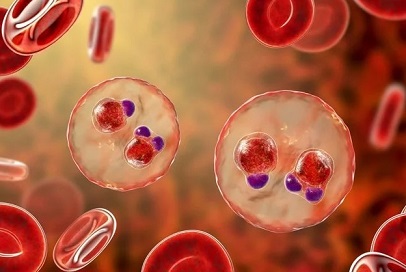
Medical News: In a shocking development, a team of scientists from Brown University has uncovered alarming mutations in malaria parasites (Plasmodium falciparum) in Ethiopia that pose a significant challenge to existing diagnostic methods and treatment regimens. The discovery of strains resistant to both antimalarial drugs and traditional diagnostic tests could jeopardize ongoing efforts to eradicate malaria in Africa. The emergence of these double-resistant parasites underscores the urgent need for innovative strategies, diagnostic tools, and treatments to combat the invisible menace. This
Medical News report delves into the alarming findings, the implications for public health, and the potential strategies to address this evolving crisis.
 New Strains Of Malaria Parasites With Mutations That Evade
New Strains Of Malaria Parasites With Mutations That Evade
Diagnostics And Drugs
The Double Threat: Mutations Evading Diagnostics and Drugs
Scientists had previously identified strains of the malaria parasite (Plasmodium falciparum) in Uganda, Tanzania, and Rwanda that exhibited resistance to commonly used antimalarial drugs. Simultaneously, in the Horn of Africa, separate strains were found to be resistant to widely employed diagnostic tests. However, the latest research from Brown University is the first to confirm the existence of a more ominous combination - parasites resistant to both treatment and detection.
According to Dr Jeffrey Bailey, the lead author of the study and an associate professor at Brown University, "Now we’re essentially seeing the worst-case scenario: parasites with the mutation that make them resistant to treatment have also picked up the chromosomal deletions that make them invisible to the diagnostic tests." This revelation poses a serious threat to malaria control and elimination efforts, making it harder to identify infected individuals and treat them effectively.
Diagnostic Challenges and Treatment Resistance
The standard diagnostic method in Africa involves rapid tests that detect specific parasite proteins in the blood. However, the newly discovered parasites have evolved to lack these proteins, rendering them invisible to conventional diagnostic tests. This stealthy behavior makes it challenging to detect infected individuals, hindering the early intervention crucial for controlling the spread of the disease.
The World Health Organization (WHO) recommends artemisinin-based combination therapy (ACT) as the primary treatment for malaria. Unfortunately, the mutations found in the Ethiopian parasites confer resistance to artemisinin, compromising the efficacy of the recommended treatment. In Ethiopia, where malaria is endemic in 75% of the country, with over 5 million cases reported annually, the implications of these mutations are dire. The Ethiopian government's goal of malaria elimination by 2030 faces significant hurdles with the emergence of these double-resistant strains.
Research Methodology and Findings
Brown University's research team, in collaboration with the Ethiopian Publi
c Health Institute and the University of North Carolina at Chapel Hill, conducted a genomic analysis of malaria parasite samples collected from three regions of Ethiopia. The study utilized next-generation sequencing techniques to identify mutations associated with both drug resistance and diagnostic evasion. The findings revealed that 8.2% of drug-resistant parasites also carried deletions of the protein-expressing gene that made them detectable by standard diagnostic tests.
In Ethiopia, the overall incidence of malaria is relatively low, but it remains endemic, posing a constant threat to 65% of the population. The discovery of these double-resistant parasites not only challenges current treatment strategies but also raises concerns about the effectiveness of existing diagnostic tools.
Unraveling the Genetic Complexity
The research involved a comprehensive genomic analysis, including the deep sequencing of key drug-resistance mutations and single nucleotide polymorphisms (SNPs) in the parasite genomes. The prevalence of the artemisinin partial-resistance kelch13 (K13) 622I mutation was found to be 8.0%, with regional variations. Importantly, these mutations were more prevalent in pfhrp2/3 non-deleted parasites compared to double-deleted ones, indicating potential misdiagnosis and less exposure to ACTs.
Population Structure and Clonal Spread
The study delves into the genetic population structure of the parasites, revealing clustering based on the K13 622I mutation and pfhrp2/3 deletion status. Identity-by-descent analysis provided evidence of recent clonal transmission and spread of the K13 622I mutation. Network analysis further illustrated the formation of related clusters among 622I mutant parasites, suggesting a localized outbreak with rapid spread.
The co-occurrence of pfhrp2/3 deletions and drug-resistance mutations, especially in key genes like pfmdr1, raises concerns about the overall efficacy of existing antimalarial drugs. The study emphasizes the need for continuous monitoring of emerging drug- and diagnostic-resistant strains to inform adaptive control strategies.
Implications for Malaria Elimination Efforts
The prevalence of these double-resistant parasites poses a formidable challenge to the goal of malaria elimination in Ethiopia and across Africa. The researchers emphasize the need for close monitoring of the spread of these strains and an improved understanding of how these mutations emerge, interact, and spread. Developing new therapies beyond artemisinin and vaccines to prevent and slow the spread of the disease becomes an urgent priority.
Dr Bailey notes, "The spread of these parasites will certainly make eliminating malaria in Ethiopia and elsewhere in Africa more difficult and will likely lead to increased cases and deaths." The study underscores the critical importance of adapting control and elimination strategies to address the evolving nature of the malaria parasite.
Genomic Surveillance Advancements and Future Outlook
The ability to conduct genomic surveillance has significantly advanced over the last decade, aided by next-generation sequencing techniques. Brown University's laboratory, led by Jeffrey Bailey, has been at the forefront of high-throughput sequencing, collaborating with research teams globally to enhance understanding and surveillance. The study highlights the ongoing efforts to build genomic surveillance capacity in Ethiopia and other parts of Africa to better monitor emerging mutations and inform effective control measures.
Conclusion
The emergence of double-resistant malaria parasites in Ethiopia represents a significant setback in the global fight against malaria. The findings from Brown University highlight the complexity of the genetic landscape and the adaptive capabilities of the malaria parasite. To address this evolving threat, there is an urgent need for collaborative efforts to develop innovative diagnostic tools, alternative treatments, and vaccines.
As Ethiopia aims for malaria elimination by 2030, the study underscores the importance of adaptive strategies that account for the dynamic nature of the parasite. Genomic surveillance, coupled with large-scale epidemiologic surveys, is crucial for gaining insights into the emergence, evolution, and spread of drug- and diagnostic-resistant parasites across Africa. The battle against malaria requires a multidimensional approach, combining scientific advancements, public health interventions, and global collaboration to overcome the challenges posed by these resilient and evolving parasites.
The study findings were published in the peer reviewed journal: Nature Microbiology.
https://www.nature.com/articles/s41564-023-01461-4
For the latest
Medical News, keep on logging to Thailand Medical News.