New Study Links Glucocorticoid Receptor Types to Breast Cancer Outcomes, Paving the Way for Personalized Treatments
Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 05, 2024 4 months, 3 weeks, 2 days, 7 hours, 26 minutes ago
Medical News: Understanding the Impact of Glucocorticoid Receptors on Breast Cancer
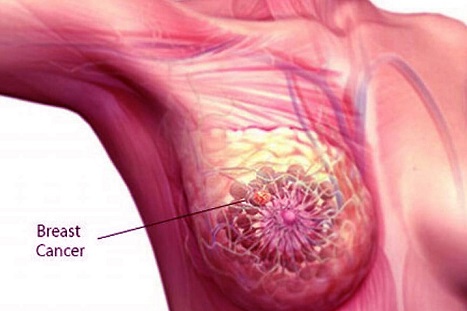
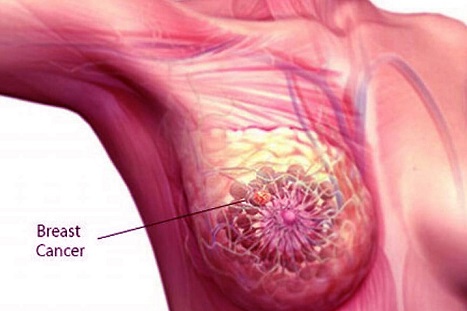
A recent study from researchers at the National Institute of Oncology, Budapest, Semmelweis University-Hungary, Eötvös Loránd University-Hungary, and ImmunoGenes-ABS Ltd-Hungary, highlights the importance of glucocorticoid receptor (GR) isoforms in breast cancer, particularly in aggressive subtypes like triple-negative breast cancer (TNBC). This
Medical News report dives into how these receptors influence cancer progression and patient survival, shedding light on potential personalized therapies.
 New Study Links Glucocorticoid Receptor Types to Breast Cancer Outcomes, Paving the
New Study Links Glucocorticoid Receptor Types to Breast Cancer Outcomes, Paving the
Way for Personalized Treatments
Glucocorticoids are commonly administered to patients undergoing chemotherapy to alleviate side effects, yet their interaction with breast cancer cells has raised questions. Glucocorticoid receptors, which are proteins on cell surfaces or within cells, respond to these glucocorticoids, but not all receptor types respond in the same way. The study focused on two isoforms: GRα and GRβ. While GRα is known to encourage cancer cell survival, GRβ behaves differently and may offer a counterbalance in breast cancer behavior, especially in subtypes that are hard to treat. The study findings suggest tailored treatment strategies for breast cancer patients based on their specific GR profiles.
Why Glucocorticoid Receptors Matter
Glucocorticoids act by binding to GRs, which can either reside in the cell’s cytoplasm or move to the nucleus upon activation. These receptors play a significant role in cellular processes, including inflammation, immune response, and even cancer progression. For patients with TNBC, this role becomes more complex. Unlike estrogen receptor-positive breast cancers, where GR expression typically indicates a better prognosis, high levels of GR in TNBC can correlate with worse outcomes.
The study reviewed two patient groups: a larger set of 194 breast cancer cases and a subset of 161 TNBC cases. By examining the cellular location and intensity of GR expression, researchers were able to classify samples based on cytoplasmic and nuclear presence of GRα and GRβ. Interestingly, cytoplasmic GRβ was linked to better survival outcomes, whereas nuclear GRα tended to worsen the prognosis.
Key Study Findings and Implications
The team’s research brought forward some critical observations about GR behavior in different breast cancer types:
-Differing Locations and Effects of GRα and GRβ: In breast cancer cells, GRα and GRβ were found in both cytoplasm and nucleus, though they showed different patterns across subtypes. In TNBC, cytoplasmic GRβ expression correlated positively with the presence of immune cells, suggesting a potential role in aiding the immune system's response to cancer. In contra
st, GRα’s presence in the nucleus was associated with shorter progression-free survival, hinting at its role in promoting cancer cell proliferation.
-GRβ as a Potential Protective Factor: The researchers observed that higher levels of GRβ in the cytoplasm correlated with improved survival in patients with TNBC. This finding is significant because it points to a protective role for GRβ, which may block the harmful effects of GRα. Moreover, the study notes that GRβ expression may increase the effectiveness of immune therapies for TNBC by potentially counteracting the cancer-supporting effects of GRα.
-Influence of Tumor Environment on GR Expression: Tumors with high lymphocyte infiltration showed higher GRβ presence, suggesting a possible link between immune system activity and receptor expression. This insight underscores the potential for immune-based therapies to interact favorably with GRβ in the tumor microenvironment, potentially halting cancer spread.
-GR Isoform Expression as a Predictor of Outcome: The study’s survival analysis showed that patients with high nuclear GRα expression had poorer outcomes. Conversely, those with substantial cytoplasmic GRβ expression experienced longer overall survival, indicating that these isoforms could help predict the prognosis for breast cancer patients, especially those with TNBC.
What the Findings Mean for Treatment Approaches
The study’s findings open doors to more personalized cancer therapies, especially for patients with aggressive cancers like TNBC. With current treatments often generalized across all breast cancer types, these insights on GR isoforms present a chance for tailored interventions. Patients with high levels of nuclear GRα could potentially benefit from reduced glucocorticoid use during chemotherapy, while those with cytoplasmic GRβ might respond better to immunotherapies or treatments that stimulate this isoform.
Moreover, this research highlights the importance of distinguishing between GRα and GRβ when diagnosing and treating breast cancer. As the study suggests, high cytoplasmic GRβ might be used as a biomarker to identify TNBC patients who could have a better prognosis or those likely to respond well to immunotherapy.
Limitations and Future Research Directions
Although these findings are promising, the study acknowledges some limitations. The complexity of GR signaling means that further research is needed to fully understand how these receptors influence cancer progression across different breast cancer subtypes. Additionally, the study relied on specific antibodies for detecting GR isoforms, and developing more accurate diagnostic tools could improve treatment precision.
Future research might focus on how manipulating GRβ expression affects immune responses in TNBC. By targeting these interactions, scientists hope to develop therapies that inhibit GRα’s cancer-promoting effects while harnessing the potential protective benefits of GRβ.
Conclusion
The study underscores the intricate role of GR isoforms in breast cancer, especially in triple-negative cases. With GRα and GRβ displaying contrasting impacts on cancer progression and patient survival, this research points toward the potential of customized treatments that consider each patient’s GR profile. In particular, the findings encourage a cautious approach to glucocorticoid use in TNBC patients with high nuclear GRα expression, as these receptors could promote cancer cell growth and spread. Conversely, cytoplasmic GRβ might hold promise as a target for immune-boosting therapies.
As research advances, targeting GR signaling pathways could become a vital strategy for tackling aggressive breast cancer types. The potential to tailor treatments based on GR status may ultimately improve outcomes and quality of life for breast cancer patients, offering a step forward in personalized oncology.
The study findings were published in the peer-reviewed International Journal of Molecular Sciences.
https://www.mdpi.com/1422-0067/25/21/11813
For the latest Breast Cancer News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/new-study-highlights-phosphatidylserine-as-a-key-biomarker-for-identifying-breast-cancer-brain-metastases
https://www.thailandmedical.news/news/breast-cancer-rates-rising-among-younger-women
https://www.thailandmedical.news/news/study-shows-that-the-phytochemical-calycosin-extracted-from-red-clover-and-astragalus-propinquus-plants-can-help-prevent-breast-cancer-metastasis