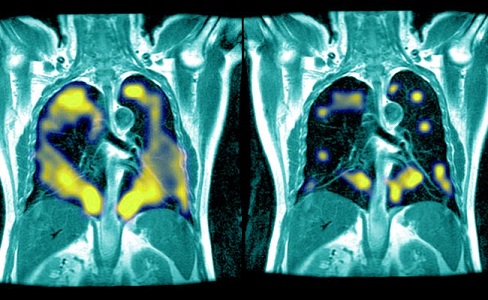
New study shows persistent pulmonary abnormalities even after three years since COVID 19 infection
Nikhil Prasad Fact checked by:Thailand Medical News Team Aug 16, 2024 7 months, 4 weeks, 15 hours, 42 minutes ago
Medical News: Persistent Lung Damage in COVID-19 Survivors: What We Know After Three Years
A new study from researchers at the Union Hospital and Wuhan Jin Yin-tan Hospital, both affiliated with the Tongji Medical College of Huazhong University of Science and Technology in Wuhan, China, reveals troubling findings about the long-term impact of COVID-19 on lung health. According to the study, a significant number of COVID-19 survivors continue to experience lung abnormalities and reduced lung function even three years after their initial infection. This
Medical News report delves into the study's findings, shedding light on what this means for the long-term health of those affected by the virus.
 New study shows persistent pulmonary abnormalities even after three years since COVID 19 infection
The Study at a Glance
New study shows persistent pulmonary abnormalities even after three years since COVID 19 infection
The Study at a Glance
The study followed 728 COVID-19 survivors who were hospitalized with varying degrees of severity during the early stages of the pandemic. These participants were meticulously monitored over three years, with follow-up assessments conducted at six months, one year, two years, and three years post-discharge. The researchers aimed to track the progression of lung abnormalities using chest computed tomography (CT) scans and pulmonary function tests, comparing these results with those of 792 non-COVID-19 controls.
Alarming Findings on Lung Function and Abnormalities
One of the most significant findings of the study is that more than a third of the COVID-19 survivors still showed signs of lung abnormalities three years after their discharge. These abnormalities included both fibrotic-like changes, which can lead to permanent lung damage, and non-fibrotic changes, which, while potentially reversible, can still cause significant respiratory issues. This article highlights that these findings underscore the long-term impact of COVID-19, especially for those who experienced severe illness.
Moreover, the study found that patients with persistent lung abnormalities were more likely to suffer from respiratory symptoms such as dyspnea (shortness of breath) and a reduced ability to exercise. The study used the six-minute walk distance (6MWD) test, which measures the distance a person can walk in six minutes, as a key indicator of lung function. The results showed that patients with lung abnormalities had significantly lower 6MWD scores compared to those whose lungs had completely healed.
Pulmonary Function: A Mixed Picture
The study also examined various pulmonary function parameters, including forced expiratory volume (FEV1) and diffusing capacity of the lung for carbon monoxide (DLCO), which is a measure of how well the lungs transfer oxygen into the blood.
The findings were somewhat mixed. While there was a general improvement in lung function over time, with some patients showing complete recovery, a significant portion of the study group continued to exhibit reduced lung function. This was especially true for those who had severe COVID-19, as indicated by their high
scores on the World Health Organization’s (WHO) seven-category severity scale during hospitalization.
Radiological Evidence of Long-Term Damage
CT scans played a crucial role in the study, revealing the persistent nature of lung abnormalities. Initially, the majority of patients exhibited ground-glass opacities (GGOs), which are cloudy areas seen on CT scans that indicate inflammation or scarring in the lungs. Over time, while some of these GGOs resolved, others progressed to fibrotic-like changes, which are much more concerning due to their potential to cause irreversible lung damage.
The study found that at the three-year mark, 36% of the survivors still had residual lung abnormalities visible on their CT scans. Among these, a subset of patients had developed fibrotic-like changes, which were associated with more severe respiratory symptoms and a greater reduction in lung function compared to those with non-fibrotic changes.
The Impact of Disease Severity
A particularly important aspect of the study was its examination of how the severity of the initial COVID-19 infection affected long-term outcomes. Not surprisingly, patients who required high-flow oxygen therapy, non-invasive ventilation, or mechanical ventilation (classified as severity scale 5-6) during their hospitalization were more likely to have persistent lung abnormalities three years later. These patients also reported higher rates of ongoing respiratory symptoms, such as cough and shortness of breath, compared to those who had less severe infections.
Implications for Long-Term Care
The findings of this study have significant implications for the long-term care of COVID-19 survivors. The persistence of lung abnormalities and the associated respiratory symptoms suggest that many COVID-19 survivors will require ongoing medical attention and possibly long-term respiratory rehabilitation. The study’s authors advocate for regular follow-up for COVID-19 survivors, especially those who experienced severe disease, to monitor and manage these long-term complications.
The study also raises concerns about the potential for these lung abnormalities to progress to more severe conditions, such as pulmonary fibrosis, a serious and often fatal lung disease. While the study did not find a high rate of progression to severe fibrosis, the presence of fibrotic-like changes in a significant number of patients underscores the need for vigilance.
Conclusion: The Long Road to Recovery
In conclusion, this study provides critical insights into the long-term effects of COVID-19 on lung health. While many patients do experience improvement over time, a significant number continue to suffer from lung abnormalities and reduced lung function even three years after their initial illness. These findings highlight the importance of long-term follow-up and care for COVID-19 survivors, particularly those who were severely affected by the virus.
The study findings were published in the peer-reviewed European Respiratory Journal.
https://erj.ersjournals.com/content/64/1/2301612
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/warning-post-covid-19-interstitial-lung-disease-worsens-over-time-and-there-is-little-hope-of-recovery
https://www.thailandmedical.news/news/individuals-who-had-covid-19-without-pneumonia-at-higher-risk-for-pulmonary-fibrosis-than-those-with-pneumonia