New Zealand Study Finds That Individuals With The Common Condition Known As Selective Immunoglobulin A Deficiency Are At Higher Risk For COVID-19 Severity!
Source: COVID-19 News - Selective Immunoglobulin A Deficiency (sIgAD) Oct 18, 2022 2 years, 6 months, 2 days, 7 hours, 42 minutes ago
COVID-19 News: Medical researchers from Auckland Hospital-New Zealand, University of Auckland-New Zealand and Wellington Hospital-New Zealand have in a new study found that selective immunoglobulin A deficiency (sIgAD) is a risk factor for severe COVID-19.
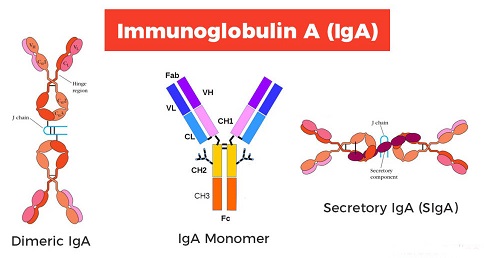
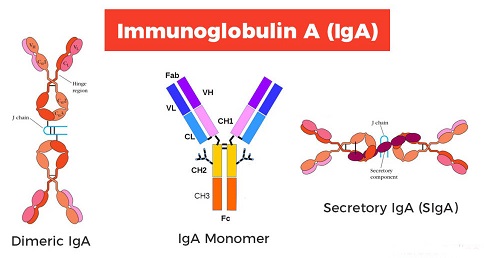
Selective IgA deficiency (sIgAD) is an immune system condition in which one lacks or don't have enough immunoglobulin A (IgA), a protein that fights infection (antibody). Individuals with Selective IgA Deficiency lack IgA, but usually have normal amounts of the other types of immunoglobulins. Selective IgA Deficiency is relatively common. Many affected people have no illness as a result. Others may develop a variety of significant clinical problems.
IgA deficiency is a common health problem that is passed down through families in about 1 in 5 cases. This means it is genetic. In rare cases, it can be caused by medicines one is taking.
Patients with selective IgA Deficiency are often considered to be at increased risk of life-threatening allergic reactions, or anaphylaxis when they receive blood products, including intravenous immunoglobulin (IVIG), that contain some IgA.
The immunoglobulin A (IgA) is an antibody blood protein that’s part of your immune system. Your body makes IgA and other types of antibodies to help fight off sickness. Having an IgA deficiency means that you have low levels of or no IgA in your blood.
IgA is found in mucous membranes, mainly in the respiratory and digestive tracts. It is also found in saliva, tears, and breastmilk. A deficiency seems to play a part in asthma and allergies. Researchers have also linked IgA deficiency to autoimmune health problems. These are health problems that cause your body’s immune system to attack your body by mistake.
Most individuals with an IgA deficiency don’t have any symptoms or health problems. Some people with an IgA deficiency are more likely to get frequent infections. These problems can include sinus, lung, and digestive infections. Some people with IgA deficiency also are more likely to have allergies. They may also have digestive and autoimmune problems such as celiac disease, rheumatoid arthritis, Graves disease, or lupus.
The SARS-CoV-2 coronavirus, the causative agent of the COVID-19 disease has wreaked havoc around the globe with hundreds of millions of individuals having been infected with the disease and more than 6.6 million have died from the infection. Many COVID-19 survivors have ongoing physical and psychiatric morbidity, which will remain for the rest of their lives.
Initially in the pandemic, it became apparent older individuals and those with comorbidities including obesity, diabetes mellitus, coronary artery disease, hypertension, renal and pulmonary disease were at increased risk of adverse outcomes. It is also clear that some immunodeficient patients, such as those with innate or T cell immune defects are at greater risk from COVID-19.
Although selective IgA deficiency (sIgAD) is generally regarded as a mild disorder, where the majority of patients are asymptomatic because of redundancy in protective immune mechanisms, worryingly recent data indicates patients with sIgAD may be at high risk of severe COVID-19.
SARS-CoV-2 gains entry primarily through the upper respiratory tra
ct mucosa, where IgA plays a critical protective role. This may underlie the vulnerability of sIgAD patients for adverse outcomes from COVID-19. This perspective highlights the need for ongoing research into mucosal immunity and improving COVID-19 treatments for patients with sIgAD.
The study findings were published in the peer reviewed Journal of Allergy and Clinical Immunology.
https://www.sciencedirect.com/science/article/pii/S2213219822010431
The study is the first to show evidence to show that selective immunoglobulin A deficiency (sIgAD) is an understated risk factor for severe coronavirus disease 2019 (COVID-19).
Considering that the incidence of Selective IgA deficiency is rather high globally, the medical community needs to pay more attention to it in this ongoing COVID-19 pandemic.
The worldwide incidence of Selective IgA deficiency varies depending on the ethnic background: 1:143 in the Arabian Peninsula, 1:163 in Spain, 1:252 in Nigeria, 1:875 in England, and 1:965 in Brazil.
https://link.springer.com/article/10.1007/s10875-009-9357-x
Selective IgA deficiency (sIgAD) is the most common type of primary immunodeficiency disorder (PID), where IgA levels remain under 0.07g/L. It is a mild disorder where the majority of patients are asymptomatic.
A number of recent studies have indicated patients with sIgAD might be at high risk of severe COVID-19 primarily because severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infects via upper respiratory tract (URT) mucosa where IgA plays a critical protective role.
Typically, there are three overlapping clinical phases of SARS-CoV-2 infection. While SARS-CoV-2 enters the nasopharynx, that phase is asymptomatic. However, patients experience fever, myalgia, and increasing dyspnea when it enters the lungs. During this time, a chest-computerized tomography (CT)scan shows a ground-glass appearance due to elevated inflammatory markers, such as interleukin 6 (IL6) and tumor necrosis factor (TNF).
Alarmingly, a few patients progress to the severe systemic phase, where their multiple organs are at risk of dysfunction, and hypoxia sometimes leads to death.
The host immune response at each SARS-CoV-2 infection phase plays a critical role in the COVID-19 outcome. Studies have shown that patients succumbing to infection often have a destructive immune response accompanied by antibody-dependent enhancement (ADE).
During the initial stages of the COVID-19 crisis, research had pointed to a steep age-related mortality gradient with high fatality rates in those over 80 years, likely because older people accumulate anti-IFN antibodies. Similarly, studies showed that patients with pre-existing medical conditions, such as obesity and hypertension, are at a higher risk of adverse COVID-19 outcomes.
However, the immunological basis of these host susceptibilities remains unclear. Also, studies have not clarified why some individuals of some ethnicities are more susceptible to poor COVID-19 outcomes.
Corresponding author, Dr Rohan Ameratunga BHB, MBChB, PhD, FRACP, FRCPA, FRCP, FRCPATH, FRCPCH, FFSc, ABMLI from the Department of Clinical Immunology at Auckland Hospital told
COVID-19 News journalists from Thailand Medical News, “It is justified to refer to chronic COVID-19 as a stalemate between SARS-CoV-2 and a suboptimal immune response. It prolongs the duration of viral shedding and points to the uncertain nature of humoral immunity in the context of pathogenic infections. Only 30% of sIgAD patients have PID-like symptoms. However, IgAD is a relatively small part of other PIDs, such as common variable immunodeficiency disorders (CVID). Studies have elucidated the genetic mechanisms governing IgAD in CVID, in which deficiencies of specific immune components (not IgA) dominate the clinical presentation.”
He further added, “In the continued absence of IgA, IgG or IgM usually compensates for mucosal immunity. However, future studies should investigate whether SARS-CoV-2 specific IgG or IgM in a patient’s saliva following COVID-19 vaccination could be of prognostic value in sIgAD patients. In addition, prospective studies may also show if in vitro T-cell responses to SARS-CoV-2 could serve as a surrogate marker for protection against COVID-19 in sIgAD patients. Together, data from these studies could help in the development of personalized medicine for COVID-19 in sIgAD patients.”
The study findings clearly show the potential vulnerability of sIgAD patients to COVID-19 and illustrates the importance of mucosal immunity research in protecting against SARS-CoV-2. A remarkable example is that since children have robust mucosal immunity, they generally suffer from mild COVID-19. Likewise, secreted IgA in breast milk protects infants against COVID-19.
The study team said that nevertheless, the immunological mechanisms governing severe COVID-19 in sIgAD remain to be defined. Future studies should investigate whether systemic autoimmunity triggered by SARS-CoV-2 triggers severe COVID-19 in sIgAD patients or lower IgA levels in URT mucosa allow SARS-CoV-2 loads to increase such that there is a risk of severe illness.
The study team also warned that although less probable, sIgAD-induced gut microbiome alterations or low gut SARS-CoV-2 neutralizing IgA contributes to a higher systemic viral load in sIgAD patients.
At present, new vaccines and therapeutics impeding SARS-CoV-2 nasal mucosal entry are in human phase III trials and might help to improve the prognosis of high-risk patients. In the future, nasal boost strategies might also prove effective. The NZACE2-Pātari project is currently pursuing ways to intercept and block SARS-CoV-2 in the nasal mucosa.
The study team refers to PIDs (Primary Immunodeficiency Disorders) as experiments of nature. SIgAD patients might enjoy good health until they contract SARS-CoV-2, like X-linked lymphoproliferative (XLP) patients until they contract Epstein-Barr virus. Also, most sIgAD patients are asymptomatic. However, monitoring their immunoglobulin levels routinely in patients admitted to hospitals with COVID-19 could help prioritize them for early treatment with monoclonal antibodies and antiviral drugs such as remdesivir. The key would be to enhance mucosal protection against SARS-CoV-2 with vaccines and therapeutics.
For the latest
COVID-19 News, keep on logging to Thailand
Medical News.