Opioids Alternatives For Joint Arthroplasty By Blocking or Temporary Destroying Nerves
Source: Thailand Medical News Nov 20, 2019 6 years, 1 month, 1 week, 2 days, 4 hours, 49 minutes ago
The excessive overuse and misuse of opioid pain medications in the US has triggered an urgent search for alternatives in an array of modalities.
Two novel approaches presented at medical meetings in the spring of 2019 appear to offer effective and long-lasting peri- and post-operative analgesia for patients undergoing total joint arthroplasty (TJA).
The first approach involves the use of ambulatory continuous femoral nerve block (ACFNB), while the other uses cryoneurolysis to temporarily destroy the nerves around the joint that deliver pain signals. Both are part of multidisciplinary pain management to effectively control pain without the use of opioids.
1.Continuous Femoral Nerve Blocks
Dr Andre P. Boezaart, MD, PhD, professor of anesthesiology and orthopaedic surgery at the University of Florida in Gainesville, presented data1 at the 2019 annual meeting of the American Academy of Pain Medicine (AAPM) on a comprehensive, collaborative multidisciplinary pain management strategy, involving nerve stimulator-guided continuous femoral nerve blocks (CFNB), which drastically reduced opioid usage and hospital stays without compromising patient satisfaction.
For his study, patients undergoing total hip arthroplasty (THA) and total knee arthroplasty (TKA) were stratified into one of four pathways: opioid-free, narcotic-naïve, standard, and chronic use. All patients (3,641 patients undergoing 4,477 procedures) undergoing THA and TKA at a tertiary academic institution were included over a 5-year period.
Typically, pain management involved collaboration between the anesthesia acute pain service and orthopedists for optimized regional anesthesia use. This included CFNB for a number of days postoperatively (a large percentage of patients went home with the blocks running), and preemptive analgesics, which included acetaminophen, ketorolac, dexamethasone, and intravenous ketamine infusion for chronic opioid users.
The study results were impressive. Among inpatient procedures, the number of prescribed opioid pills decreased by 45.8%. In the outpatient setting, the drop was even greater at 56.7%. Patient satisfaction did not change, but actually increased slightly. Hospital length of stay decreased from 3.2 to 1.5 days. The rate of patient discharges to a skilled nursing facility decreased from approximately 40% to around 10%, while re-admission rates also decreased from 4.5% to 3.7%. Zero percent of the re-admissions were pain-related.
Ambulatory nerve stimulator-guided CFNB formed the central component of this multimodal pain strategy. For TKA, anesthesiologists performed the CFNB in combination with iPACK (infiltration between popliteal artery and capsule of the knee); CFNB combined with posterior capsule injections were used in the THA patient category.
Dr. Boezaart told
Thailand Medical News that while ultrasound guidance is sometimes used to ensure the right location for placing the needle for CFNB, generally the femoral nerve is very easy to find with nerve stimulation only.
In his practice, nerve stimulation is used exclusively for the catheter placement. He explained that for the block to work days after catheter placement and in order to prevent secondary block failure, “you have to have the tip of the catheter in the correct compartment of the fascia layers around the nerve. It has to be in the compartment deep to the circumneu
rium (previously termed ‘paraneurium’), and this collagen membrane is not visible with ultrasound. The only way to reliably and consistently place the catheter deep to the circumneurium is to use a stimulating catheter,” he said. He added that secondary block failure usually occurs “if the motor responses disappear or get weaker upon advancement of the catheter. It means the catheter is not in the correct compartment, and the block will fail in subsequent days.”
The main reason that CFNB is not used more often, according to Dr. Boezaart, has to do with a fear among clinicians of causing muscle weakness in quadriceps. However, “this fear is not founded in science or reality.” While quadriceps weakness is a problem with knee and hip surgery, “it is caused by arthrogenic muscle inhibition (AMI), which starts long before the surgery and is mainly due to the disease itself and the surgery.” AMI can last up to 18 months after surgery, whereas “CFNB has very little or no long-lasting influence on quadriceps weakness. If anything, the block could inhibit the AMI pathways and even enhance quadriceps muscle function recovery,” he explained.
2.Cryoneurolysis
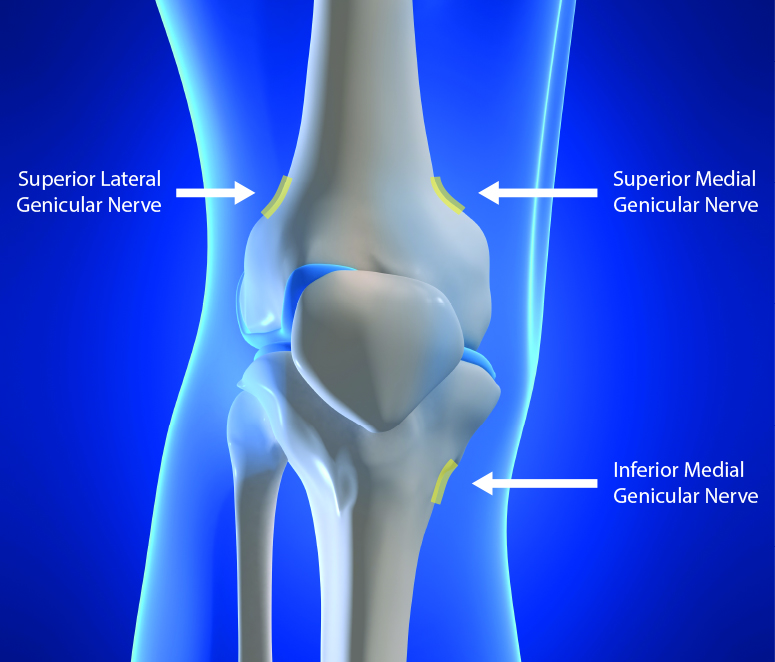
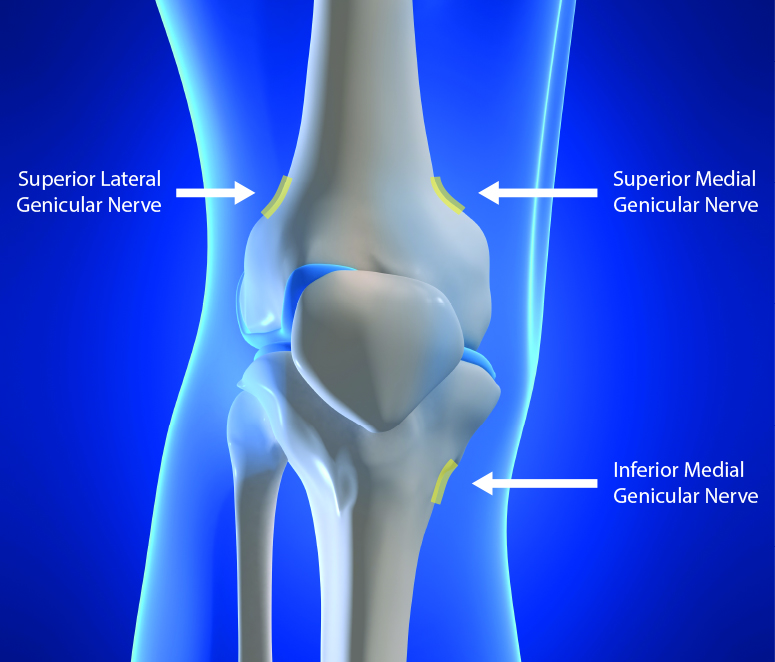
Dr William Mihalko, MD, PhD, professor at the Campbell Clinic Department of Orthopedic Surgery and Biomedical Engineering at the University of Tennessee Health Science Center in Memphis, TN, discussed results2 using the iovera system for pain management during and after TKA at the 2019 annual meeting of the American Academy of Orthopaedic Surgeons (AAOS). The iovera system used cryoneurolysis to cause temporary destruction of targeted nerve fibers, which in turn prevented pain signaling. Specifically, cryoneurolysis caused the degeneration of the axon and myelin sheath, which are responsible for pain signaling. The affected axons and myelin sheath take time to regenerate, producing a long-lasting nerve block.
Dr. William Mihalko presented data from 125 patients scheduled to undergo a primary TKA. Patients were randomized to control and cryoneurolysis groups. Pain management before, during, and after surgery was the same for both groups, with the exception of cryoneurolysis. In the treatment group, the iovera therapy was administered to the superficial genicular nerve 3 to 7 days prior to surgery.
Dr. Mihalko told
Thailand Medical News,“Using landmarks, it is not difficult to learn the technique. I trained my
physician assistants with very little difficulty.”
The key endpoint, daily morphine equivalents (DME),a measure of opioid use was significantly lower at 72 hours for patients receiving cryoneurolysis (12.1 mg vs 17.8 mg). DME was also lower for this group at six weeks (4.5 mg vs 6.3 mg) and 12 weeks (2.3 mg vs 3.5 mg). In addition, patients who had iovera therapy were three times less likely to take opioids six weeks after surgery compared with the control group. Patients in the treatment group also had significant reductions in pain scores from the baseline at 72 hours and at 12 weeks.
Participants in the study treatment group also reported faster improvement in flexion compared to the control group over the post-operative period. Patient perception appears to be positive as well. “A few patients were certain it was much less painful than their previous TKA, if they had their other knee done in the past,” Dr. Mihalko told
Thailand Medical News.
As a component of a multimodal approach to pain management for TKA, this technique appears to have a measurable impact on pain relief, reducing patient opioid use after surgery. “I am seeing my patients recover more quickly, with less pain,” Dr. Mihalko concluded.
References:
1. Boezaart AP, et al. A comprehensive protocol for post-operative pain control in elective total joint arthroplasty drastically reduces opioid prescriptions: A review of prescribing practices and outcome. Presented at: American Academy of Pain Medicine (AAPM) 2019 Annual Meeting, March 8, 2019, in Denver, CO.
2. Mihalko W, et al. Cryoanalgesia: A Path to an Opioid-Free TKA, Pre-op Through Rehab. Presented at: American Academy of Orthopaedic Surgeons (AAOS) 2019 Annual Meeting, March 13, 2019, in Las Vegas, NV.