Post-COVID-19 Vaccination Emergence Of Kaposi Sarcoma In Immunocompetent Individuals!
Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 26, 2024 1 year, 2 months, 4 hours, 38 minutes ago
COVID-19 News: The advent of COVID-19 vaccines has been hailed as a significant milestone in the global fight against the pandemic. However, amidst the widespread vaccination campaigns, emerging reports of unexpected adverse events have garnered attention from the scientific community. One such occurrence that has recently surfaced is the development of Kaposi Sarcoma (KS) following COVID-19 vaccination in immunocompetent individuals. This unexpected association challenges existing paradigms and underscores the need for comprehensive investigation into the potential links between vaccination, viral reactivation, and oncogenesis.
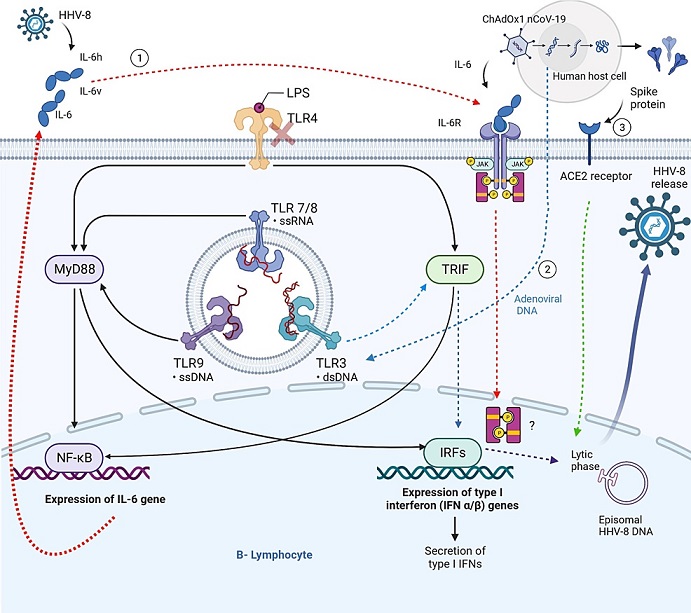
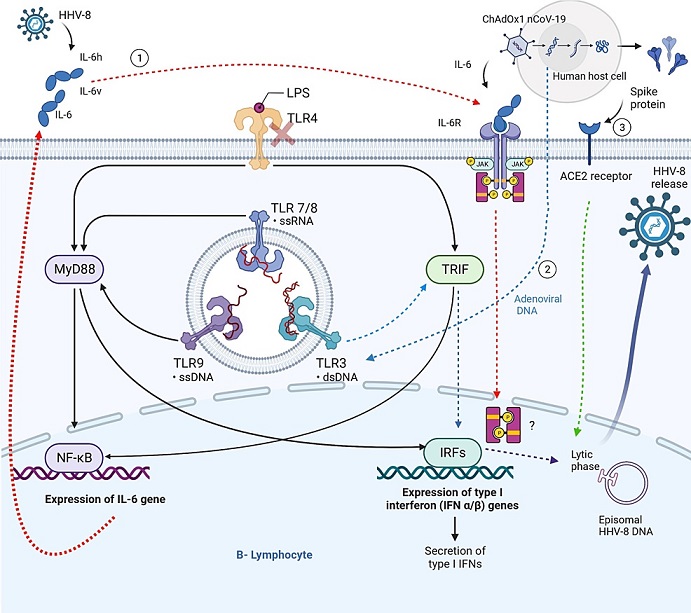 Hypothesized mechanisms underlying reactivation of HHV-8 by the ChAdOx1 nCoV-19 vaccine.
Human herpes virus 8 (HHV-8) engages the immune system, leading to the synthesis of human interleukin 6 (IL-6h) by the host and viral interleukin 6 (IL-6v) produced from viral DNA. The ChAdOx1 nCoV-19 vaccine stimulates the production of interleukin-6 (IL-6). The Toll-like receptor (TLR) pathway facilitates the production of interleukin-6 (IL-6) by activating nuclear factor-kappa B (NF-kB) transcription factors through the involvement of MyD88 and TRIF. Interleukin-6 (IL-6) forms a complex with its specific receptor, initiating the activation of the lytic phase of Human Herpes virus 8 (HHV-8). Nevertheless, the mechanism of this activation via the JAK/STAT3 pathway remains speculative and lacks conclusive evidence. Adenoviral DNA or RNA transcripts have the potential to stimulate intracellular Toll-like receptors (TLRs) 3, 7, 8, and 9. This activation, facilitated by TRIF and IRFs, leads to the initiation of the HHV-8 lytic phase. The binding of spike proteins to the ACE receptor results in the reactivation of the lytic phase of HHV-8. ACE receptor (angiotensin-converting enzyme), HHV-8 (herpes virus 8), interferon-regulatory factor, IL-6h (human Interleukin 6) IL-6v (viral IL-6), LPS (Lipopolysaccharides), MyD88 (Myeloid differentiation primary response 88), TLR (toll-like receptor), TRIF (TIR-domain-containing adapter-inducing interferon-β).
Hypothesized mechanisms underlying reactivation of HHV-8 by the ChAdOx1 nCoV-19 vaccine.
Human herpes virus 8 (HHV-8) engages the immune system, leading to the synthesis of human interleukin 6 (IL-6h) by the host and viral interleukin 6 (IL-6v) produced from viral DNA. The ChAdOx1 nCoV-19 vaccine stimulates the production of interleukin-6 (IL-6). The Toll-like receptor (TLR) pathway facilitates the production of interleukin-6 (IL-6) by activating nuclear factor-kappa B (NF-kB) transcription factors through the involvement of MyD88 and TRIF. Interleukin-6 (IL-6) forms a complex with its specific receptor, initiating the activation of the lytic phase of Human Herpes virus 8 (HHV-8). Nevertheless, the mechanism of this activation via the JAK/STAT3 pathway remains speculative and lacks conclusive evidence. Adenoviral DNA or RNA transcripts have the potential to stimulate intracellular Toll-like receptors (TLRs) 3, 7, 8, and 9. This activation, facilitated by TRIF and IRFs, leads to the initiation of the HHV-8 lytic phase. The binding of spike proteins to the ACE receptor results in the reactivation of the lytic phase of HHV-8. ACE receptor (angiotensin-converting enzyme), HHV-8 (herpes virus 8), interferon-regulatory factor, IL-6h (human Interleukin 6) IL-6v (viral IL-6), LPS (Lipopolysaccharides), MyD88 (Myeloid differentiation primary response 88), TLR (toll-like receptor), TRIF (TIR-domain-containing adapter-inducing interferon-β).
While the case study covered in this
COVID-19 News report covers the occurrence of Kaposi Sarcoma in an immunocompetent individual following the ChAdOx1 nCoV-19 (AstraZeneca) vaccine by researchers from Dermatological Institute of Jalisco, Guadalajara-Mexico, Mexican Institute of Social Security, Campeche-Mexico and McGill University, Montreal-Canada, there has been other case studies of emergence of Kaposi Sarcoma after other COVID-19 vaccines as well including those by Pfizer and Moderna in both immunocompetent as well as immunocompromised individuals.
https://www.sciencedirect.com/science/article/pii/S2451993623001949
https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-021-00620-9
quot;https://www.anaisdedermatologia.org.br/en-covid-19-infection-vaccines-potential-triggers-articulo-S0365059623000235">https://www.anaisdedermatologia.org.br/en-covid-19-infection-vaccines-potential-triggers-articulo-S0365059623000235
https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(24)00021-5/fulltext
https://www.sciencedirect.com/science/article/pii/S0365059623000235
https://link.springer.com/article/10.1007/s15010-023-02121-9
Background on Kaposi Sarcoma
Kaposi sarcoma, initially described by Moritz Kaposi in 1872, has long been recognized as a multifaceted disease with distinct clinical presentations and epidemiological patterns. Traditionally, KS has been associated with specific demographic groups, notably older men of Mediterranean descent. However, recent years have witnessed a shifting landscape, with KS cases increasingly reported among individuals of diverse ethnic backgrounds, including those of Latin American origin and who are immunocompetent.
https://www.jaad.org/article/S0190-9622(21)01740-0/abstract
Classic KS typically manifests as sporadic lesions on the skin, most commonly affecting the lower extremities. Historically, KS has been strongly linked to immunosuppression, particularly in the context of HIV/AIDS. However, the emergence of KS in immunocompetent individuals has raised intriguing questions about alternative pathogenic mechanisms and potential triggers.
Case Presentation
The reported case involves a 73-year-old man with a notable medical history of dyslipidemia and arterial hypertension, who presented to the dermatology clinic with a perplexing constellation of symptoms. On examination, the patient exhibited a 2×3x1 cm infiltrated plaque and multiple violaceous and red nodules on the dorsal aspect of his right hand. Remarkably, the lesions were asymptomatic and had emerged approximately one week after the patient received the third dose of the ChAdOx1 nCoV-19 (AstraZeneca) vaccine.
Over the ensuing two months, the KS lesions exhibited progressive growth and evolution, ultimately culminating in the development of a palpable tumor. Notably, the patient lacked Mediterranean ancestry, denied engagement in sexual activity with men, and had no prior history of COVID-19 infection. HIV testing yielded negative results, further complicating the diagnostic puzzle.
Histopathological examination confirmed the diagnosis of classic KS, with positive immunohistochemistry analysis for CD34 and HHV-8.
Treatment involved a multidisciplinary approach, with cryotherapy selected as the primary modality. The patient underwent three sessions of cryotherapy, spaced three weeks apart, resulting in complete clearance of the lesions. While the clinical outcome was favorable, the underlying mechanisms driving the development of KS following COVID-19 vaccination remained enigmatic.
Exploring Potential Mechanisms: Unraveling the Connection
The emergence of KS following COVID-19 vaccination raises intriguing questions about the interplay between viral reactivation, immune modulation, and oncogenesis. Extensive literature searches failed to yield prior reports linking KS to COVID-19 vaccination, underscoring the novelty and significance of the reported case.
Central to understanding this phenomenon is the role of Kaposi sarcoma-associated herpesvirus (KSHV), a known etiological agent implicated in the pathogenesis of KS. Studies have elucidated various mechanisms through which viral reactivation may occur, particularly in the context of immunomodulatory stimuli such as vaccination.
The ChAdOx1 nCoV-19 vaccine, characterized by its adenovirus vector platform, presents a unique avenue for investigating the potential interactions between vaccination and viral oncogenesis. Notably, spike proteins of SARS-CoV-2, the virus causing COVID-19, have been implicated in the reactivation of the lytic phase of KSHV. The presence of DNA encoding proteins in the vaccine formulation raises intriguing possibilities regarding the activation of latent viral reservoirs and subsequent oncogenic transformation.
Two primary pathways for viral reactivation have been proposed, each shedding light on distinct aspects of the pathogenic cascade. Firstly, the adenovirus vector-induced expression of pro-inflammatory cytokines, particularly interleukin-6 (IL-6), may play a pivotal role in KSHV reactivation. Studies have demonstrated a direct correlation between IL-6 levels and the activation of KSHV lytic replication, suggesting a mechanistic link between vaccine-induced inflammation and viral oncogenesis.
Secondly, the adenovirus vector's DNA strands may serve as potent triggers for Toll-like receptor (TLR) activation, particularly TLR7 and TLR8. These intracellular receptors play a crucial role in innate immune sensing and may contribute to the reactivation of latent viral reservoirs. Notably, the spatial distribution of vaccine components and their interaction with immune cells may further modulate the inflammatory milieu, providing a conducive environment for viral replication and oncogenic transformation.
Furthermore, syncytia formation induced by the SARS-CoV-2 spike protein represents an intriguing avenue for exploring the mechanistic underpinnings of KS development post-vaccination. The increased fusion of nuclei from different lymphocytes may enhance the probability of KSHV DNA interaction, particularly in cells harboring latent viral reservoirs. Thus, syncytia formation may serve as a mechanistic link between viral antigen exposure and oncogenic transformation, further complicating the pathogenic landscape.
Conclusion: Towards Comprehensive Understanding and Vigilance
In conclusion, the emergence of Kaposi Sarcoma following COVID-19 vaccination underscores the complexity of viral oncogenesis and the need for ongoing vigilance. While this case represents a singular occurrence, it highlights the intricate interplay between vaccination, viral reactivation, and oncogenic transformation. Comprehensive understanding of the underlying mechanisms is imperative for refining vaccination strategies and mitigating potential risks.
Moving forward, continued surveillance and comprehensive investigation are essential for elucidating the pathogenic cascade and identifying potential risk factors. Collaborative efforts between clinicians, researchers, and public health authorities are crucial for advancing our understanding of vaccine-associated outcomes and ensuring the safety and efficacy of vaccination campaigns.
As we navigate the evolving landscape of COVID-19 vaccination, a proactive approach to surveillance and research is paramount. By unraveling the complexities of viral oncogenesis, we can better anticipate and mitigate potential adverse events, ensuring the continued success of global vaccination efforts in combating the pandemic.
The case study was published in the peer reviewed journal: Cureus.
https://www.cureus.com/articles/202213-sporadic-kaposi-sarcoma-following-a-covid-19-vaccine-mere-coincidence-or-something-more#!/
For the latest
COVID-19 News, keep on logging to Thailand Medical News.