Pregnancy And COVID-19: Canadian Led Study Shows That Maternal Immune Cells Transmits SARS-CoV-2 To The Placenta
Source: Pregnancy And COVID-19 Oct 01, 2020 5 years, 2 months, 3 weeks, 6 days, 1 hour, 21 minutes ago
Pregnancy And COVID-19: Canadian researchers from the University of Toronto, Sinai Health Systems-Toronto, Lunenfeld-Tanenbaum Research Institute-Toronto along with support from the University of Minas Gerais-Brazil have in a new study found that maternal immune cells actually help to spread the SARS-CoV-2 coronavirus to the placenta.

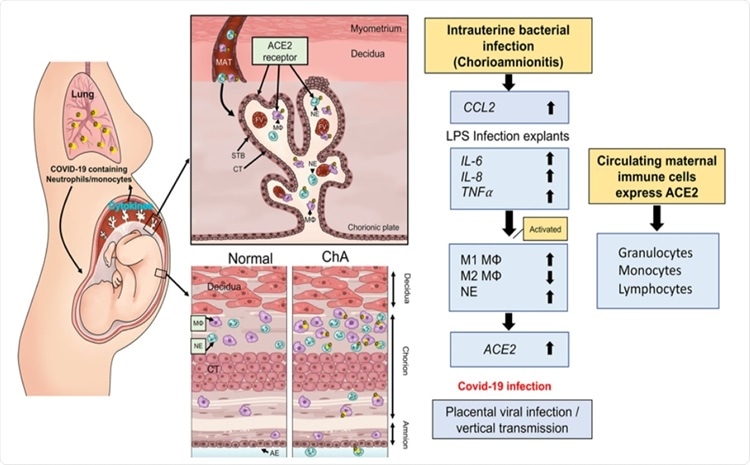
In the study, the researchers provided evidence that under conditions of intrauterine infection/inflammation there is an influx of ACE2 expressing neutrophils and macrophage into the placenta. The team suggest that this is a potential mechanism by which maternal-fetal vertical transmission could occur in COVID 19 infected pregnancies.
The research findings are published on a preprint server and have yet to be peer reviewed.
https://www.medrxiv.org/content/10.1101/2020.09.27.20201590v2
So far thousands of pregnant women have been infected with the novel coronavirus but cases of transmission of the infection from the infected mother to the baby are rare and to date, there have been almost no reports of deaths in the neonates infected with the virus.
There is conflicting data as to whether SARS-CoV-2 can be transmitted to the fetus through the placenta in women with COVID-19.
Early reports of obstetric and neonatal outcomes of pregnant women from China with COVID-19 suggested that SARS-CoV-2 infection in pregnancy results in limited neonatal infection
https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003195 and
https://www.ajog.org/article/S0002-9378(20)30197-6/fulltext
However, an increasing number of studies reporting neonatal cases with congenital or intrapartum infection. So far, 10 infants with SARS-CoV-2 infection meet these criteria based on a classification system defined by Shah et al.
https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/aogs.13870
Notably, a clinical case report revealed that a neonate born to a COVID-19 infected pregnant woman was tested positive for SARS-CoV-2 after 36 hours of postnatal life, which meets the criteria of intrauterine transmission (Blumberg et al.2020).
https://pubmed.ncbi.nlm.nih.gov/32161941/ and
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7356079/
Also, in one preterm pregnancy case, the baby tested negative for COVID-19 at birth, and positive 24 hours later.
https://pubmed.ncbi.nlm.nih.gov/32304114/
Three other neonates showed increased immunoglobulin M (IgM) antibodies specific to COVID19 at birth
https://pubmed.ncbi.nlm.nih.gov/32215589/
There is also a growing body of evidence demonstrating infe
ction of the placental membrane and the villous trophoblasts, a recent electron microscopy study has demonstrated the presence of SARS-CoV-2 in placental STB and Baud et al have reported a case of SARS-CoV-2 positivity in the placental submembranes and cotyledons together with mixed inflammatory infiltration and funicity in pregnant woman in the second trimester. In this case, placental infection of SARS-CoV-2 was confirmed by the virologic findings from specimen obtaining from the fetal surface.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219376/ and
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7193526/
The study team from Canada and Brazil collaborated to explore the possibility of perinatal transmission of the SARS-COV-2 coronavirus from pregnant mothers to their babies and the risk of preterm birth.
To date there are only a handful of documented cases of transmission of the infection from the mother to baby or vertical transmission of COVID-19.
The study team explained that some research have shown that there is a possibility of infiltration of inflammatory content in the placenta intervillous region. This infiltrate contains neutrophils and monocyte macrophages among pregnant women with SARS-CoV-2 infection. These cells express activation markers. Studies have also shown the potential for transmission of SARS-CoV-2 from an infected mother to her fetus/neonate before birth.
At present, there is little information regarding the risk of complications in pregnancy raised due to COVID-19. However, some reports have shown a higher risk of maternal and neonatal complications in COVID-19 positive mothers. The risk of preterm births, for example, rose to 20 percent, and infection in the neonates was around 6 percent.
The researchers say that the immune system stands between the mother and the fetus, and when the immune system of the mother is disrupted, as in the case of bacterial infection, both the mother and the baby are at risk of other infections, such as viruses.
Hence immune cells that lie between the fetus and the mother play a critical role in a successful pregnancy. At the initial stage of the pregnancy, it remodels the uteroplacental circulation, for example, and in the third trimester, it leads to the inflow of maternal peripheral monocytes and immune cells into the uterus that leads to the initiation of the delivery process and labor.
It is already known that the SARS-CoV-2 coronavirus enters the cells through angiotensin-converting enzyme 2 (ACE2). The SARS-CoV spike protein interacts with the host receptor ACE2 using the subunit S1 and then fuses the viral and host membranes through subunit S2.
Importantly the fetal heart, kidneys, liver, lung, and placenta also contains the ACE2 receptors, and the levels of ACE2 is high in the syncytiotrophoblast layer (STB) and villous stroma between the fetus and the mother.
The study team hypothesized that if the mother had an infection, her maternal macrophage and neutrophils would be activated, and they would target the uterus. If the ACE2 is expressed on these cells then they have the potential to transport the SARS-CoV-2 virus to the placenta and thus raise the risk of placental infection followed by COVID-19 in the baby.
The study team collected information from the placentas from pregnancies that had complications such as chorioamnionitis (ChA). They noted that these placentas had a high expression of ACE2 mRNA.
The team also collected second-trimester placentas and treated them with LPS (Lipopolysaccharide from the outer membrane of Gram-negative bacteria) led to an acute increase in cytokine expression followed by ACE2 mRNA.
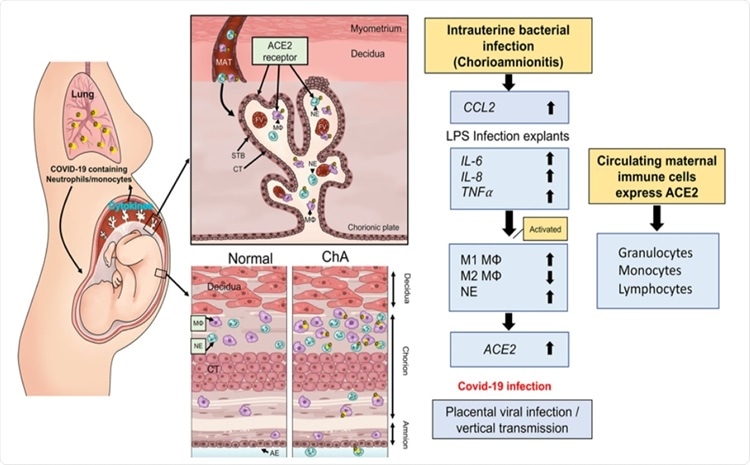 Schematic model by which maternal immune cells could bring SARS-CoV-2 to the placenta and increase risk of vertical transmission in pregnancies complicated by intrauterine infection. Intrauterine bacterial infection, such as occurs in chorioamnionitis (ChA), leads to increased expression and release of chemokine/cytokines by the placenta that in turn induce activation of maternal immune cells, notably M1 macrophage and neutrophils. These cells then target the sites of infection in the placenta/fetal membranes. Subsets of these immune cells express the SARS-CoV-2 cell entry protein, ACE2, and thus are targets for viral uptake in women infected with SARS-CoV-2. The virus may then be hypothetically transported to the placenta increasing the potential for vertical transmission of the virus to the fetus. MAT= maternal blood, FV= fetal vessel, MΦ= M1 macrophage, NE= neutrophil, STB= syncytiotrophoblast, layer CT= cytrophoblast.
Schematic model by which maternal immune cells could bring SARS-CoV-2 to the placenta and increase risk of vertical transmission in pregnancies complicated by intrauterine infection. Intrauterine bacterial infection, such as occurs in chorioamnionitis (ChA), leads to increased expression and release of chemokine/cytokines by the placenta that in turn induce activation of maternal immune cells, notably M1 macrophage and neutrophils. These cells then target the sites of infection in the placenta/fetal membranes. Subsets of these immune cells express the SARS-CoV-2 cell entry protein, ACE2, and thus are targets for viral uptake in women infected with SARS-CoV-2. The virus may then be hypothetically transported to the placenta increasing the potential for vertical transmission of the virus to the fetus. MAT= maternal blood, FV= fetal vessel, MΦ= M1 macrophage, NE= neutrophil, STB= syncytiotrophoblast, layer CT= cytrophoblast.
Subsequently all the ACE2 protein in the placenta was collected in the syncytiotrophoblast, in fetal blood vessels. There was a rise in M1/M2 macrophage and neutrophils in the villous stroma of the placenta.
It was observed that M1 macrophage and neutrophils rose in numbers in the placenta of ChA pregnancies. Maternal peripheral immune cells, including granulocytes and monocytes, were found to contain ACE2 mRNA and protein.
The study team concluded “The study findings show that the presence of an intrauterine bacterial infection results in the infiltration of ACE2 expressing maternal macrophage and neutrophils into and across the placental tissues.”
The study team said that COVID19 positive pregnancies, especially those with chorioamnionitis, had ACE2 positive immune cells.
The team added “These ACE2 expressing immune cells have the potential to transport the SARS-CoV-2 coronavirus to the placenta in cases of COVID-19 infection in pregnancy and increase the risk of placental infection and vertical transmission of the virus to the fetus.”
For more on
Pregnancy And COVID-19, keep on logging to Thailand Medical News.