Source : Thailand Medical News Oct 26, 2019 5 years, 5 months, 1 week, 23 hours, 36 minutes ago
There is growing evidence that the addition of triglyceride-lowering medication and lifestyle changes may be valuable in diabetes management.
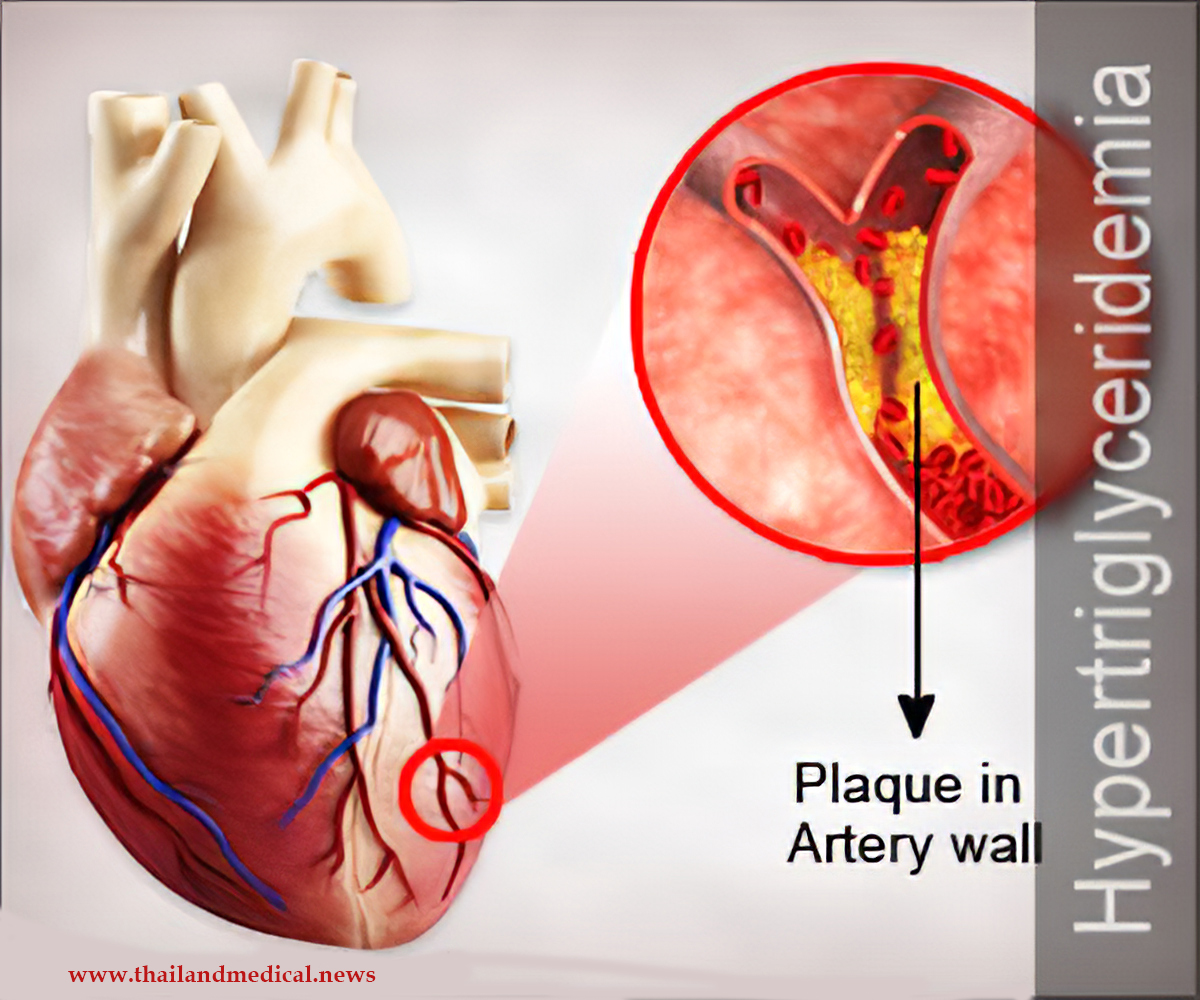
Due to growing evidence that moderate
hypertriglyceridemia contributes to
cardiovascular risk, there is a need to look at the impact of lowering triglycerides in patients with the
diabetic dyslipidemia phenotype.
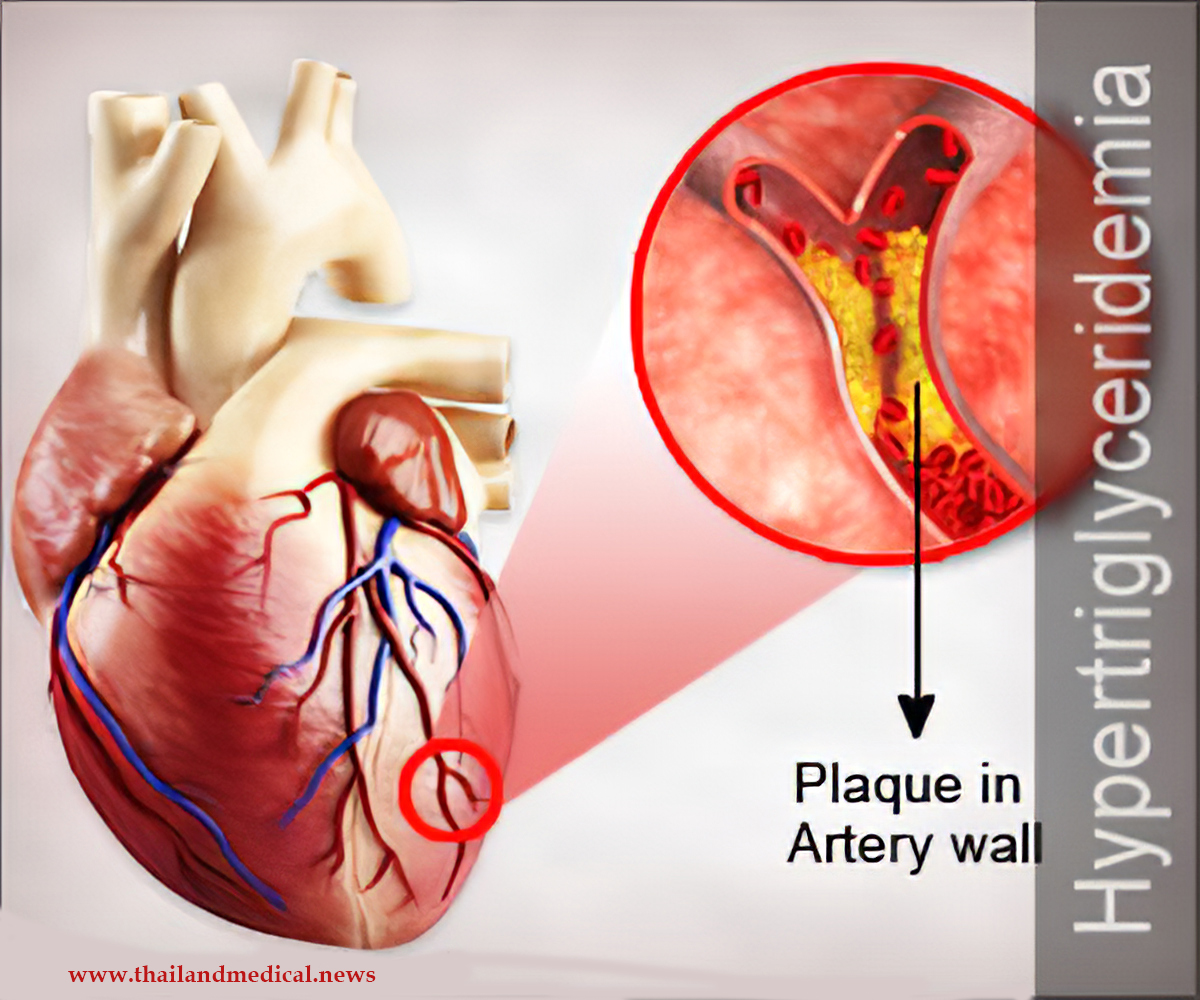
The condition of
diabetic dyslipidemia is characterized by a pattern of high triglycerides and low high-density lipoprotein (HDL) cholesterol, which is most frequently observed in people with type
2 diabetes.
1 It may present several years before the onset of hyperglycemia and could be a treatable risk factor for subsequent
cardiovascular disease.
2
Typically, triglycerides provide energy storage in adipose cells and transport esterified fatty acids when circulating in chylomicrons, very low-density lipoproteins (VLDL), and lipoprotein remnants.
1 Hypertriglyceridemia is defined by excess triglycerides in the blood as a result of metabolic dysfunction, arising from surplus VLDL production or inefficient lipolysis. Inefficient lipolysis occurs when HDL and low-density lipoprotein (LDL) particles undergo triglyceride enrichment.
1 HDL particles lose apolipoproteins that aid in the assembly, transport, and metabolism of lipids, while LDL particles become smaller and more atherogenic.
1,3
The conventional presentation of
diabetic dyslipidemia involves low levels of HDL, which has a protective role against heart disease through antioxidative and anti-inflammatory mechanisms.
2 The dynamic interaction of high triglyceride levels and low HDL therefore yields an effect that contributes to
cardiovascular risk.
The correlation between triglycerides and coronary heart disease (CHD) is quite strong. Raised serum triglycerides herald the development of
type 2 diabetes mellitus, particularly when associated with other features of metabolic syndrome or CHD, and once diabetes has developed they continue to predict CHD risk, often independent of other risk factors.
In multivariate analyses, including individual factors that are associated with
hypertriglyceridemia including obesity, elevated cholesterol levels, and glucose intolerance, somewhat attenuates the
cardiovascular risk associated with elevated triglycerides. Still, risk for CHD is substan
tial in
hypertriglyceridemia: fasting triglyceride levels of 230.09 to 398.23 mg/dL are linked to double the risk for CHD and fasting levels of 398.23 to 796.46 mg/dL are linked to a 9-fold increase in CHD risk.
2
There is growing evidence that the addition of triglyceride-lowering medication and lifestyle changes may be valuable in
diabetes management. The interaction between
hypertriglyceridemia and low HDL seems to further increase the risk associated with
heart disease. While evidence suggests that depressed HDL levels alone are a risk factor for the development of
diabetes and
cardiovascular disease, HDL catabolism is heightened in a hypotriglyceridemic state.
2
Individuals with
diabetes who have good glycemic control often have higher than normal HDL levels, and the occurrence of
hypertriglyceridemia in this population does not seem to have a clear relationship to cardiovascular risk. This further illustrates the burden of low HDL levels on patients with
hypertriglyceridemia and high cardiometabolic risk.
Effect Of Insulin On Triglycerides
Glucose-lowering medications, such as insulin, have a range of effects on triglycerides.
1 Insulin suppresses the enzymes responsible for releasing nonesterified fatty acids from triglycerides (thereby releasing glyceride as a byproduct), but low insulin levels activate them.
1 Excess nonesterified fatty acids released under the state of insulin deficiency/resistance increase triglyceride production in the liver, driving the development of
diabetic dyslipidemia.
2
As such it can be seen that managing glycemic control in patients with
diabetic dyslipidemia has varying effects on
hypertriglyceridemia. While insulin may reduce circulating triglycerides, there is no consistent effect on cholesterol, and low HDL levels reduce the ability to further metabolize lipids.
1 With this in mind, treatments like pioglitazone, a strong insulin sensitizer, are the best option for lowering triglycerides while raising HDL levels.
1
Certain clinical trials have failed to show beneficial effects of intensive glycemic control on
cardiovascular outcomes, whereas others have demonstrated that the favorable effects of glycemic control on
cardiovascular health may actually relate to lipoprotein metabolism rather than changes to glycemia.
2
Treatment That Lower Triglycerides
A recent meta-analysis of trials shows that lowering triglycerides benefits a specific subset of patients who demonstrate patterns consistent with
diabetic dyslipidemia.
1 In the case of high-risk lipid phenotypes, treatment should ideally target both high triglyceride and low HDL levels to reduce
cardiovascular risk in these patients.
The most effective manner to treating
hypertriglyceridemia is lifestyle modification, specifically exercise and weight loss with a very low-fat diet and total abstinence from alcohol. It may be beneficial to refer these patients to a lipid specialist and medical dietician.
3 In addition to lifestyle changes, specific adjunctive therapies should be considered in the treatment of
diabetic dyslipidemia, such as fibrates, omega-3 fatty acids, and niacin.
Drugs like Fibrates (fenofibrate and gemfibrozil) are potent triglyceride-lowering agents that are often used as add-on therapy to statins. Several studies have shown that fibrates can substantially reduce triglycerides by 30% to 50%, as well as decrease negative cardiovascular outcomes.
1 Omega-3 fish oil supplements can augment fibrate treatment to lower triglycerides by suppressing VLDL production.
1
Vitamin B3 or niacin is also indicated in
dyslipidemias that involve high triglycerides and low LDL, especially in extended release formulations, which minimize the risk for hepatotoxicity. Niacin therapy has been shown to lower triglycerides by approximately 25% and raise HDL by almost 30%.
3 It is important to note that while some dedicated cholesterol medications can reduce
cardiovascular risk, they may worsen triglyceride levels, and care should be taken in prescribing these to patients with
diabetic dyslipidemia.
3
Thailand Medical News recommends that diabetic patients frequently get their lipid profile screenings done on a regular basis and also check with their physician or endocrinologist to assess their conditions and see the need to take any drugs to prevent cardiovascular incidences associated with
diabetes.
References:
1. Alexopoulus AS, Qamar A, Hutchins K, Crowley MJ, Batch BC, Guyton JR. Triglycerides: emerging targets in diabetes care? Review of moderate hypertriglyceridemia in diabetes. Curr Diab Rep. 2019;19(4):13.
2. Schofield JD, Liu Y, Rao-Balakrishna P, Malik RA, Soran H. Diabetes dyslipidemia. Diabetes Ther. 2016;7(2):203-219.
3. Pejic RN, Lee DT. Hypertriglyceridemia. J Am Board Fam Med. 2006;19(3):310- 316.