Recent Rituximab Or Cancer Chemotherapy Drugs Use Linked To Increased Risk Of Post-COVID-19 Pulmonary Fibrosis!
COVID-19 News:
Pulmonary fibrosis, a condition characterized by the destruction of lung tissue, has been observed as a common consequence of severe COVID-19 infection. It can lead to significant morbidity and mortality among patients recovering from the virus. As researchers explore potential factors that contribute to the development of post-COVID-19 pulmonary fibrosis, they have turned their attention to medications used before COVID-19 infection. Among these drugs are amiodarone, cancer chemotherapy, corticosteroids, and rituximab.
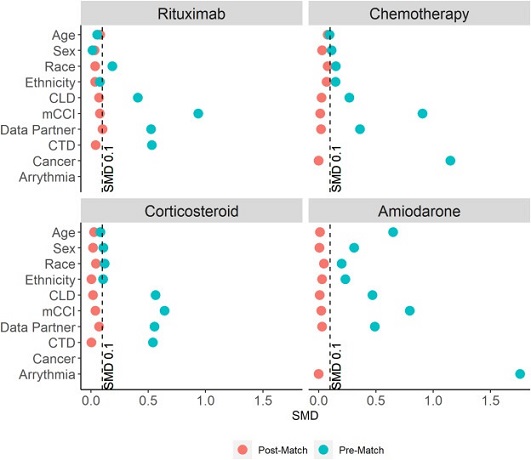
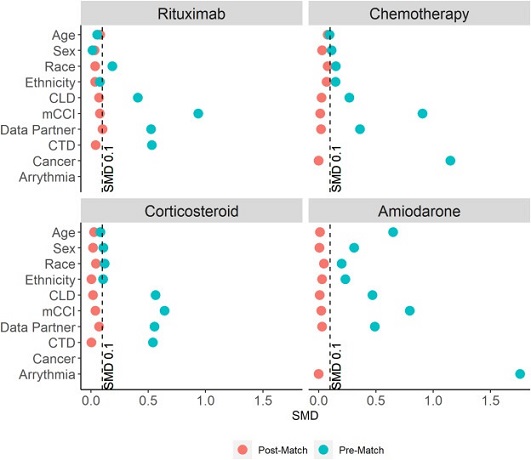 Covariate balance pre- and post- propensity score matching, 60-day cohort
Covariate balance pre- and post- propensity score matching, 60-day cohort
Understanding their association with
pulmonary fibrosis risk could help guide treatment decisions and improve patient outcomes.
The Study
To investigate this association, researchers from the University of Chicago-USA analyzed data from the National COVID-19 Cohort Collaboration (N3C) Data Enclave, which aggregated COVID-19 data across the United States. The study focused on adults hospitalized between January 2020 and July 2022, excluding those with pre-existing pulmonary fibrosis. The researchers used propensity scores to match pre-COVID-19 drug-exposed and unexposed cohorts (1:1) based on factors known to influence pulmonary fibrosis risk.
Findings
The study included 452,951 hospitalized adults with
COVID-19, among whom pulmonary fibrosis incidence was found to be 1.1 per 100-person-years. The primary analysis included 277,984 hospitalized adults with COVID-19, and all drug-exposed cohorts were well-matched to unexposed cohorts. The results showed that rituximab use before COVID-19 infection was associated with a 2.5 times higher risk of post-COVID-19 pulmonary fibrosis. Similarly, cancer chemotherapy was linked to a 1.6 times increased risk, and corticosteroids had a 1.2 times increased risk. On the other hand, amiodarone did not show a significant association with post-COVID-19 pulmonary fibrosis.
Pulmonary fibrosis has been a growing concern among COVID-19 survivors, with substantial lung damage observed in those hospitalized with acute respiratory distress syndrome. This study sheds light on the potential role of certain medications in influencing the risk of post-COVID-19 pulmonary fibrosis. Rituximab, an immunosuppressive medication used to treat autoimmune disorders, was found to have a significant association with pulmonary fibrosis risk. It is postulated that rituximab's immunosuppressive effects might disrupt the body's ability to clear viral infections, leading to an increased risk of fibrosis.
Similarly, cancer chemotherapy, known for its immunosuppressive effects, was also linked to an increased risk of post-COVID-19 pulmonary fibrosis. The immunosuppression caused by cancer chemotherapy might r
esult in viral reactivation in recovered COVID-19 patients, prolonging inflammation and heightening the risk of pulmonary fibrosis.
Corticosteroids, commonly used to manage inflammatory lung conditions, showed a marginal increase in pulmonary fibrosis risk when compared to matched controls. Again, the immunosuppressive nature of corticosteroids might play a role in promoting the fibrotic process that occurs in COVID-19 patients, leading to an increased risk of pulmonary fibrosis.
Interestingly, amiodarone, despite being strongly linked to pulmonary fibrosis on its own, did not show a significant association with an increased risk of post-COVID-19 pulmonary fibrosis. This suggests that the risk of pulmonary fibrosis associated with amiodarone might not be further amplified by COVID-19 infection.
Implications
The findings of this study have significant implications for clinicians and patients managing COVID-19 and its aftermath. Understanding the potential risks associated with specific medications can guide treatment decisions and help healthcare providers weigh the benefits and risks of using certain drugs. While the study provides valuable insights into the association between medication use and post-COVID-19 pulmonary fibrosis, researchers acknowledge that other factors may also contribute to this complex relationship.
Conclusion
In conclusion, this study highlights the potential risk posed by certain medications, specifically rituximab and cancer chemotherapy, for the development of post-COVID-19 pulmonary fibrosis. As the global burden of COVID-19 continues, understanding and managing potential post-infection complications, such as pulmonary fibrosis, become crucial for providing comprehensive care to patients. Further research is needed to delve deeper into the mechanisms underlying these associations and to identify strategies to mitigate the risk of pulmonary fibrosis in COVID-19 survivors.
The study findings were published in the peer reviewed journal: The Lancet Regional Health – Americas
https://www.thelancet.com/journals/lanam/article/PIIS2667-193X(23)00140-0/fulltext
For the latest COVID-19 News, keep on logging to
Thailand Medical News.