Researchers Develop New Treatment Protocol For Drug Resistance Advanced Bile Duct Cancer
Source: Thailand Medical News Jan 15, 2020 5 years, 3 months, 1 week, 4 days, 22 hours, 42 minutes ago
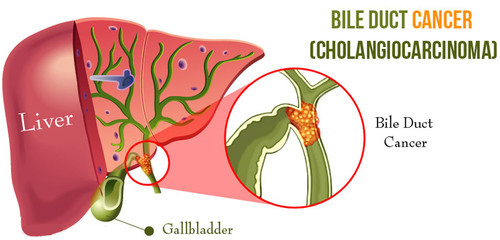
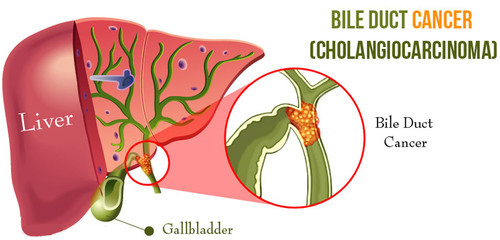
A research led by medical oncologists at The Ohio State University Comprehensive Cancer Center, Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC—James) shows how resistance to a promising targeted drug develops in patients with a rare, lethal
cancer of the
bile ducts called
cholangiocarcinoma.
The research, reported in the journal
Molecular Cancer Therapeutics, also suggests that adding another drug at the time of progression might re-sensitize tumor cells to the initial drug, called an
FGFR inhibitor.
Study leader Dr Sameek Roychowdhury, MD, Ph.D., a medial oncologist and researcher at the OSUCCC—James told
Thailand Medical News, "While the majority of patients with
FGFR-positive
cholangiocarcinoma benefit from new
FGFR inhibitors in clinical trials, most patients unfortunately develop
cancers resistant to the drugs. We believe that this study is an important step in understanding
drug resistance, and improving the treatment of this and other
cancers caused by abnormal
FGFR gene mutations."
Research findings also suggest that monitoring fragments of circulating tumor DNA for acquired mutations that cause
resistance to
FGFR inhibitors may reveal the presence of
resistance mutations and mark the time a patient should begin taking the additional drug, an
mTOR inhibitor.
Typically, the successful treatment of
cholangiocarcinoma is challenging because the disease is usually diagnosed at an advanced stage that has a five-year survival rate of 2%. Patients diagnosed earlier also have low five-year survival due to high rates of disease recurrence. Abnormal activation of the
FGFR gene happens in 15 to 20% of people with
cholangiocarcinoma, and
FGFR inhibitors show effectiveness in 70 to 80% of those patients until
resistance develops. There are six studies of
FGFR inhibitors in clinical trials at the OSUCCC—James.
First author Dr Melanie Krook, Ph.D., a postdoctoral fellow in Roychowdhury's lab added, "A better understanding of how treatment
resistance develops and how to prevent it is critical for improving the treatment of
cholangiocarcinoma and other
cancers caused by
FGFR mutations. Our research findings suggest that cholangiocarcinoma patients treated with an
FGFR targeted therapy could potential benefit from combination therapies with other drugs such as
mTOR inhibitors. Additional laboratory studies are needed to identify the optimal lead strategies for this combination."
<
br />
In the research, Dr Roychowdhury, Dr Krook and colleagues examined the
FGFR (fibroblast growth factor receptor) gene in the
cancer cells of a
cholangiocarcinoma patient who died after experiencing disease progression and developing
resistance to the
FGFR inhibitor infigratinib.
The team identified two acquired
FGFR mutations in the patient's tumor cells that conferred
resistance to
FGFR inhibitors.
They then used
cancer cell lines to learn that the mutations led to activation of the
mTOR biochemical pathway. This enabled the
cancer cells to grow even in the presence of
FGFR inhibitors. Adding an
mTOR inhibitor to the cells restored their sensitivity to
FGFR inhibitors.
Significant findings from the study include:
-Two acquired
FGFR2 mutations, p.E565A and p.L617M, were shown to drive
resistance to the
FGFR inhibitor infigratinib.
-The p.E565A mutation upregulates the
mTOR signaling pathway, which desensitizes
cholangiocarcinoma cell lines to
infigratinib and other
FGFR inhibitors.
-A drug that inhibited the
mTOR pathway restored the sensitivity of the cells to
infigratinib and other
FGFR inhibitors.
Dr Roychowdhury concluded,"Overall, our findings suggest that an
mTOR inhibitor administered at the time of progression may re-sensitize tumor cells to an
FGFR inhibitor in patients who develop
resistance to these agents."
Reference : Melanie A. Krook et al. Efficacy of FGFR inhibitors and combination therapies for acquired resistance in FGFR2-fusion cholangiocarcinoma, Molecular Cancer Therapeutics (2020). DOI: 10.1158/1535-7163.MCT-19-0631