Researchers From Cedar-Sinai Discover That Parkinson’s Disease May Start Before Birth And Are Also Developing Potential New Treatment
Source: Thailand Medical News Jan 29, 2020 5 years, 11 months, 4 weeks, 10 hours, 47 minutes ago
Individuals who develop
Parkinson’s disease before age 50 may have been born with disordered brain cells that went undetected for decades, according to new Cedars-Sinai research. The new research points to a drug that potentially might help correct these disease processes.
Typically,
Parkinson’s occurs when brain
neurons that make
dopamine, a substance that helps coordinate muscle movement, become impaired or die. Symptoms, which get worse over time, include slowness of movement, rigid muscles, tremors and loss of balance. In most cases, the exact cause of
neuron failure is unclear, and there is no known cure.
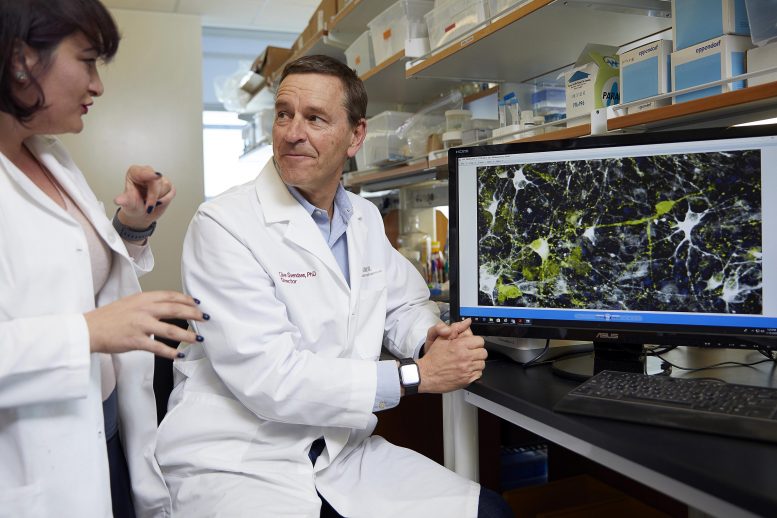
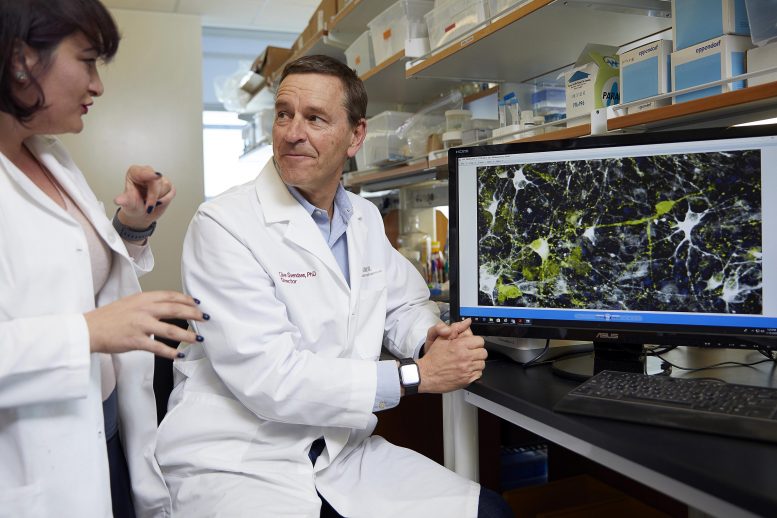 Dr Clive Svendsen, Ph.D., director of the Cedars-Sinai Board of Governors Regenerative
Dr Clive Svendsen, Ph.D., director of the Cedars-Sinai Board of Governors Regenerative
Medicine Institute, right, and Nur Yucer, Ph.D., a project scientist, discuss a microscope
image of dopamine neurons. Credit: Cedars-Sinai
More than 430,000 people in the U.S. and 3.1 million people globally are diagnosed with
Parkinson’s each year, and the incidence is rising. Although most patients are 60 or older when they are diagnosed, about 10% are between 21 and 50 years old. The new study, published in the journal
Nature Medicine, focuses on these young-onset patients.
Dr Michele Tagliati, MD, director of the Movement Disorders Program, vice chair and Professor in the Department of Neurology at Cedars-Sinai told
Thailand Medical New, “Young-onset
Parkinson’s is especially heartbreaking because it strikes people at the prime of life. This exciting new research provides hope that one day we may be able to detect and take early action to prevent this disease in at-risk individuals.”
For the study, the research team generated special stem cells, known as
induced pluripotent stem cells (
iPSCs), from cells of patients with young-onset
Parkinson’s disease. This process involves taking adult blood cells “back in time” to a primitive embryonic state. These
iPSCs can then produce any cell type of the human body, all genetically identical to the patient’s own cells. The team used the
iPSCs to produce
dopamine neurons from each patient and then cultured them in a dish and analyzed the
neurons’ functions.
Dr Clive Svendsen, PhD, director of the Cedars-Sinai Board of Governors Regenerative Medicine Institute and Professor of Biomedical Sciences and Medicine at Cedars-Sinai added, “Our technique gave us a window back in time to see how well the
dopamine neurons might have functioned from the very start of a patient&rs
quo;s life,”. Dr Svendsen was the study’s senior author.
The medical researchers detected two key abnormalities in the
dopamine neurons in the dish:
-An accumulation of a protein called
alpha-synuclein, which occurs in most forms of
Parkinson’s disease.
- Massive malfunctioning lysosomes, cell structures that act as “trash cans” for the cell to break down and dispose of proteins. This malfunction could cause
alpha-synuclein to build up.
Dr Svendsen further added, “What we are seeing using this new model are the very first signs of young-onset
Parkinson’s. It appears that
dopamine neurons in these individuals may continue to mishandle
alpha-synuclein over a period of 20 or 30 years, causing
Parkinson’s symptoms to emerge.”
The medical investigators also used their
iPSC model to test a number of drugs that might reverse the abnormalities they had observed. They found that that one drug,
PEP005, which is already approved by the Food and Drug Administration for treating precancers of the skin, reduced the elevated levels of
alpha-synuclein in both the
dopamine neurons in the dish and in laboratory mice.
The new drug also countered another abnormality they found in the patients’
dopamine neurons ie elevated levels of an active version of an enzyme called protein kinase C ,although the role of this enzyme version in
Parkinson’s is not clear.
Dr Tagliati said the team plans for the next steps, to investigate how
PEP005, currently available in gel form, might be delivered to the brain to potentially treat or prevent young-onset
Parkinson’s. The team also plans more research to determine whether the abnormalities the study found in
neurons of young-onset
Parkinson’s patients also exist in other forms of
Parkinson’s.
Dr Shlomo Melmed, MB, ChB, executive vice president of Academic Affairs and Dean of the Medical Faculty at Cedars-Sinai commented, “This research is an outstanding example of how physicians and investigators from different disciplines join forces to produce translational science with the potential to help patients. This important work is made possible by the dual leadership of Cedars-Sinai as both a distinguished academic institution and an outstanding hospital.”
Reference: “iPSC modeling of young-onset Parkinson’s disease reveals a molecular signature of disease and novel therapeutic candidates” by A. H. Laperle, S. Sances, N. Yucer, V. J. Dardov, V. J. Garcia, R. Ho, A. N. Fulton, M. R. Jones, K. M. Roxas, P. Avalos, D. West, M. G. Banuelos, Z. Shu, R. Murali, N. T. Maidment, J. E. Van Eyk, M. Tagliati and C. N. Svendsen, 27 January 2020, Nature Medicine.
DOI: 10.1038/s41591-019-0739-1