Source: Thailand Medical News Feb 04, 2020 6 years, 5 days, 10 hours, 5 minutes ago
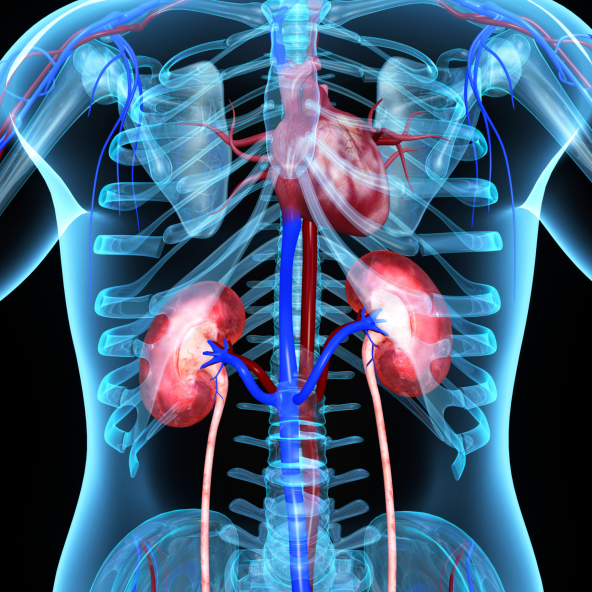
Individuals with chronic kidney disease have a higher risk for heart disease and heart-disease death. Now, for the first time in humans, research led by Dr Navkaranbir Bajaj, M.D., of the University of Alabama at Birmingham, has identified a pathological change that appears to link
kidney disease to progressive
heart disease.
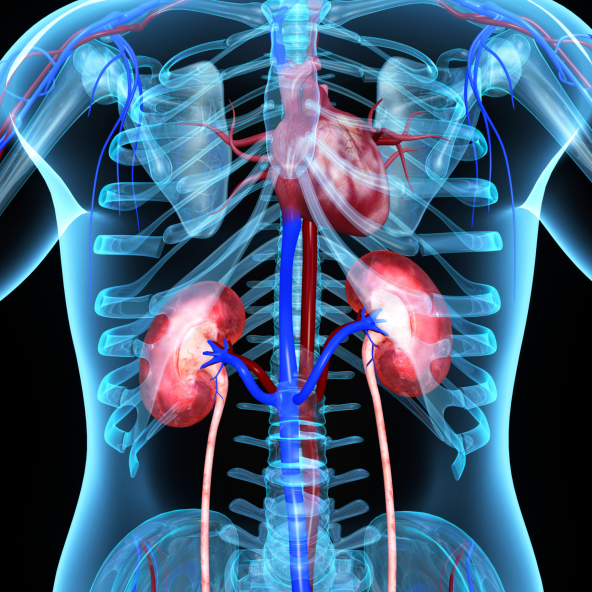
The new discovery offers a potential treatment target, which could have wide benefit because 14 percent of the U.S. adult population has chronic
kidney disease. The research is published in the journal
Circulation, with Dr Bajaj, a UAB Assistant Professor in the Division of Cardiovascular Disease, Department of Medicine and Department of Radiology as first author.
Dr Bajaj told
Thailand Medical News, "I am now collaborating with other UAB researchers to figure out how we can target therapeutics to help these patients."
Coronary microvascular dysfunction, or
CMD is the identified pathological change say Dr Bajaj along with research colleagues at Harvard Medical School. CMD is decreased blood flow in the small blood vessels inside the heart muscle that provide oxygen and fuel to feed the pumping heart.
Normally in healthy hearts, visualized postmortem, these blood vessels look like a tight filigree network that fills the heart muscle tissue. A diseased postmortem heart has lost much of this network. In living patients, however, those small blood vessels inside the heart muscle cannot be visualized; blood flow scans of living patients visualize only the larger, exterior coronary arteries. So Dr Bajaj and colleagues needed an indirect way to gauge
CMD.
That new measure is
coronary flow reserve, or
CFR, which Dr Bajaj and colleagues measured via positron emission tomography.
CFR is the maximum increase in blood flow through the coronary arteries above the normal resting volume. Dr Bajaj, a cardiologist who trained at UAB, did his advanced imaging fellowship at Brigham and Women's Hospital in Boston, before returning to UAB in 2018.
It was observed that In a longitudinal study of 352 patients with chronic
kidney disease, all with healthy heart function as measured by ejection fraction and none with signs of overt coronary artery disease, the researchers measured
CFR and also measured signs of subclinical heart dysfunction via deformation analysis with echocardiograms. The patients were then followed a median of 4.4 years for major adverse cardiac events. A total of 108 patients had such major events, including death and hospitalization for non-fatal
heart attack or
heart failure.
The medical researchers found that
CMD was a significant predictor of abnormal mechanics of the left ventricle, the heart's major pumping chamber and a significant predictor of clinical risk of
adverse cardiovascular outcomes.
A new statistical model called mediation analysis examined the relationship between impaired kidney function and
heart disease. It showed that
CMD accounted for 19 to 24 percent of left ventricle diastolic dysfunction, 19 to 42 percent of left ventricle systolic dysfunction and 32 percent of major adverse cardiovascular events.
These observed significant associations "provide important new evidence that the development of severe
coronary microvascular dysfunction likely signals the transition from physiological to pathological left ventricle remodeling that increases the risk of heart failure and death in patients with chronic
kidney disease," the study said. "To the best of our knowledge, our study is the first and largest to comprehensively explore these associations and to suggest a possible pathway to the development of uremic cardiomyopathy in individuals without overt ischemic
heart disease."
Reference
: Navkaranbir S. Bajaj et al, Coronary Microvascular Dysfunction, Left Ventricular Remodeling, and Clinical Outcomes in Patients With Chronic Kidney Impairment,
Circulation (2019).
DOI: 10.1161/CIRCULATIONAHA.119.043916