Researchers In Singapore Warn That SARS-CoV-2 Can Lead To Creutzfeldt-Jakob Disease In Some Post COVID Individuals Presenting With Psychiatric Symptoms
Thailand Medical News Team Aug 08, 2023 1 year, 8 months, 1 week, 3 days, 17 hours, 43 minutes ago
In a startling revelation, researchers in Singapore have sounded the alarm about a potential connection between COVID-19 and the development of
Creutzfeldt-Jakob Disease (CJD) in certain individuals who have recovered from the virus. This revelation comes as part of an ongoing investigation into the intricate interplay between the SARS-CoV-2 virus and the human body, shedding light on a previously unrecognized aspect of the ongoing pandemic.
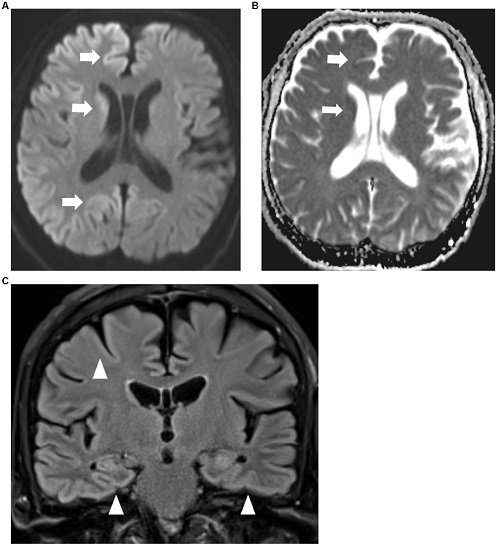
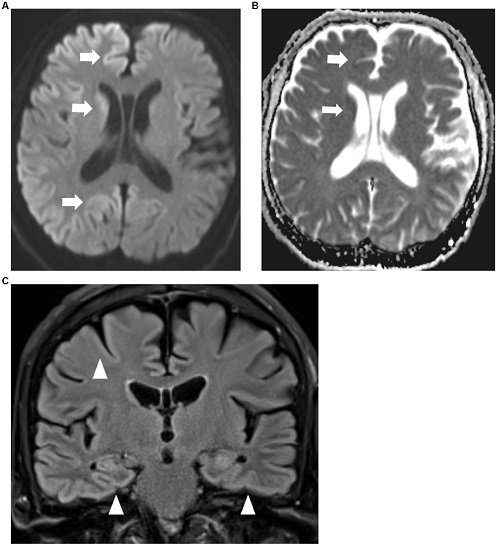 MRI brain axial diffusion weighted imaging sequence (A) with corresponding apparent diffusion co-efficient sequence (B) showing restricted diffusion of both cerebral cortices and caudate nuclei (arrows) which are more prominent on the right. (C) MRI brain coronal FLAIR sequence showing FLAIR hyperintensities of bilateral cerebral cortices (arrowheads).
Creutzfeldt-Jakob Disease
MRI brain axial diffusion weighted imaging sequence (A) with corresponding apparent diffusion co-efficient sequence (B) showing restricted diffusion of both cerebral cortices and caudate nuclei (arrows) which are more prominent on the right. (C) MRI brain coronal FLAIR sequence showing FLAIR hyperintensities of bilateral cerebral cortices (arrowheads).
Creutzfeldt-Jakob Disease, a rare and sinister neurodegenerative disorder, has long been a subject of intrigue within the medical community due to its rapid progression and fatal consequences. This disorder is characterized by the accumulation of misfolded prion proteins in the central nervous system (CNS), leading to a host of devastating cognitive and motor deficits.
The disease typically presents with neurocognitive deficits, ataxia, and abnormal movements, making it a daunting adversary to both patients and medical practitioners alike.
However, what has raised eyebrows is the reported case of a 70-year-old man in Singapore whose initial manifestations of
Creutzfeldt-Jakob Disease surfaced shortly after contracting COVID-19. The man's journey began with symptoms of anxiety and short-term memory loss, which emerged mere weeks after experiencing a mild bout of COVID-19. Over time, his condition deteriorated, culminating in parkinsonism and, tragically, akinetic mutism. The patient's battle ended five months after the onset of symptoms, leaving researchers puzzled by the apparent temporal relationship between COVID-19 infection and the emergence of neurodegenerative symptoms.
The case underscores the importance of delving into the intricate mechanisms that underlie both COVID-19 and neurodegenerative disorders. The initial symptoms of anxiety and memory loss, though alarming, were initially attributed to the aftermath of COVID-19 infection and the psychological toll it can take. This case serves as a powerful reminder that psychiatric symptoms can serve as early indicators of deeper neurodegenerative processes.
The intertwining threads of this narrative lead to the question of how COVID-19 might contribute to the development of
Creutzfeldt-Jakob Disease. One plausible avenue of exploration centers on the intricate relationship between the virus and the central nervous system. SARS-CoV-2, the virus responsible for COVID-19, can directly infiltrate the CNS through multiple routes, including the olfactory epithelium and the bloodstream. This invasion can potentially compromise the blood-brain barrier, giving rise to neuroinflammation - a phenomenon that has been increasingly associated with COVID-
19.
The immune response elicited by the virus can trigger an array of inflammatory cytokines, leading to the disruption of the blood-brain barrier and consequent neuroinflammation. This scenario mirrors the pathological process observed in neurodegenerative disorders like
Creutzfeldt-Jakob Disease, where the accumulation of misfolded proteins triggers an inflammatory response within the brain. The potential connection becomes even more intriguing when considering the role of microglia and astrocyte - essential players in maintaining CNS homeostasis and regulating inflammation.
Microglia, the resident immune cells of the CNS, play a vital role in modulating inflammation and maintaining the CNS environment. However, their role becomes complex when prion diseases like
Creutzfeldt-Jakob Disease enter the picture. The accumulation of prion proteins triggers microglial activation, which, in a bid to clear the harmful proteins, can transition from an anti-inflammatory to a pro-inflammatory state. This shift can escalate the neuroinflammatory response, exacerbating the progression of neurodegeneration.
Astrocytes, meanwhile, take on the task of regulating neurovascular function and maintaining the integrity of the blood-brain barrier. They also contribute to neuroinflammation when activated in response to external stimuli, such as a viral infection. The parallels between the inflammatory responses in both COVID-19 and
Creutzfeldt-Jakob Disease hint at a potential crossroads, where the immune response to the virus might inadvertently contribute to the neuroinflammatory processes associated with neurodegeneration.
A particularly intriguing element of this puzzle lies in the 'S1' spike protein present on the surface of SARS-CoV-2. Emerging evidence suggests that this protein may be involved in the aggregation of various proteins within the brain, including prion proteins. This aggregation can mimic the pathological changes observed in prion diseases and Alzheimer's disease. Furthermore, the 'S1' spike protein contains domains that bear resemblance to prion-like structures, potentially contributing to systemic amyloidosis and systemic inflammation.
Despite the compelling narrative that emerges from this case and the intriguing potential connections between COVID-19 and
Creutzfeldt-Jakob Disease, researchers remain cautious.
While the temporal relationship between the two cannot be ignored, it is essential to exercise prudence in drawing definitive conclusions. The case report serves as a clarion call for heightened vigilance when assessing individuals who exhibit psychiatric symptoms and cognitive decline post-COVID-19 infection. Such symptoms could be indicative of an underlying neurodegenerative process that warrants thorough investigation.
The study findings were published in the peer reviewed journal: Frontiers In Neurology.
https://www.frontiersin.org/articles/10.3389/fneur.2023.1239576/full
For the latest about
Creutzfeldt-Jakob Disease, keep on logging to Thailand Medical News.