Researchers Warn That Flaws In Many Surgical Operating Theaters Increase Risk Of COVID-19 Infection!
Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 29, 2024 1 year, 9 months, 3 weeks, 4 hours, 17 minutes ago
COVID-19 News: The COVID-19 pandemic has underscored the importance of safety measures in healthcare settings, particularly in surgical operating theaters. A recent study conducted by engineers at New York University Abu Dhabi (NYUAD) that is covered in this
COVID-19 News report, has revealed critical flaws in traditional ventilation systems used in operating theaters, posing an increased risk of COVID-19 infection for surgical teams and patients. The findings shed light on the limitations of existing ventilation systems and propose a flexible and innovative ventilation framework to enhance safety during surgical procedures.
 Researchers Warn That Flaws In Many Surgical Operating Theaters Increase Risk Of COVID-19 infection!
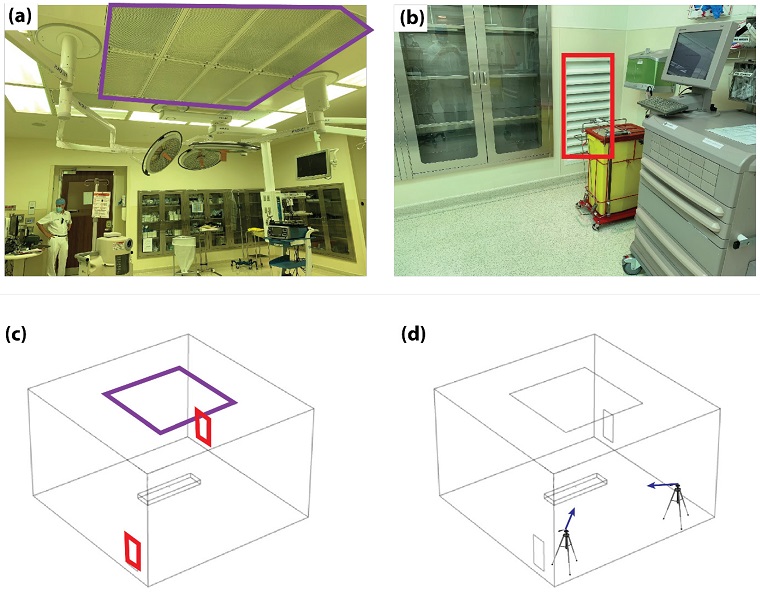
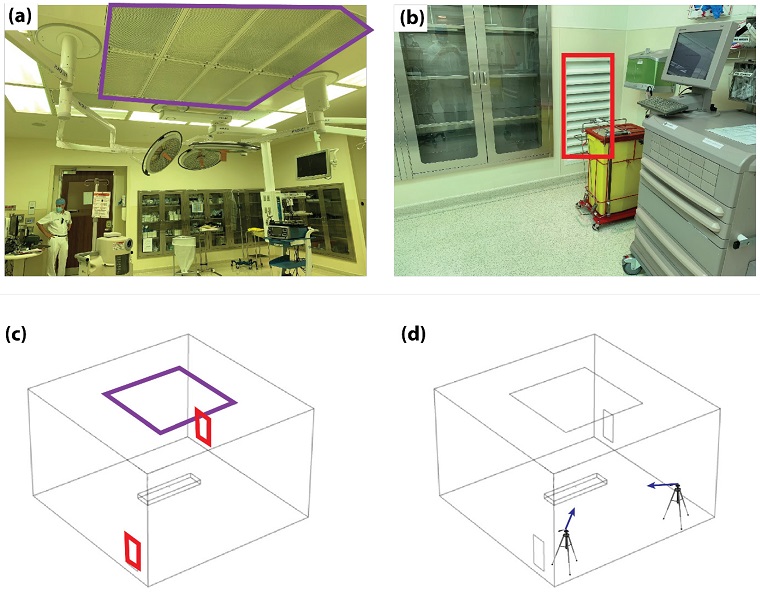
Experimental and numerical setups. (a) Image of the real operating room with the inlet duct highlighted (purple square). (b) Corner of the operating theater with one of the outlet ducts highlighted (red square). (c) Corresponding CFD domain geometry with the inlet (purple square) and outlet ducts (red squares) highlighted. (d) Representative schematic highlighting the positions (tripods) and directions (blue arrows) of the particle tracking cameras.
Current Challenges in Operating Room Ventilation
Researchers Warn That Flaws In Many Surgical Operating Theaters Increase Risk Of COVID-19 infection!
Experimental and numerical setups. (a) Image of the real operating room with the inlet duct highlighted (purple square). (b) Corner of the operating theater with one of the outlet ducts highlighted (red square). (c) Corresponding CFD domain geometry with the inlet (purple square) and outlet ducts (red squares) highlighted. (d) Representative schematic highlighting the positions (tripods) and directions (blue arrows) of the particle tracking cameras.
Current Challenges in Operating Room Ventilation
Traditionally, ventilation systems in operating theaters have been designed to protect patients from airborne contamination and surgical site infections. These systems create an airflow pattern that pushes air away from the operating table, reducing the risk of contamination in the sterile surgical zone. However, the study conducted by NYUAD engineers indicates that these ventilation systems may inadvertently circulate aerosolized pathogen-carrying particles, especially those generated by powered surgical tools. This unintended circulation exposes the surgical team to potential infections, contradicting the common practice of placing support staff away from the patient and towards the operating room walls.
Study Methodology and Key Findings
The research, titled "Ventilation-Based Strategy to Manage Intraoperative Aerosol Viral Transmission in the Era of SARS-CoV-2," utilized a combination of computational modeling and experimental procedures in active operating theaters. Collaborating with surgeons from Cleveland Clinic Abu Dhabi, the NYUAD research team, led by Mohammad Qasaimeh, director of the University's Advanced Microfluidics and Microdevices Laboratory, identified shortcomings in existing ventilation systems. Their research highlighted that traditional ventilation systems tend to spread germs around, particularly towards the perimeter of the operating theater, putting supporting surgical staff at a higher risk.
Key Flaws Identified In The Study
The study identified several existing flaws in traditional ventilation systems used in operating rooms, which inadvertently contribute to the circulation of aerosolized pathogen-
carrying particles. These flaws increase the risk of COVID-19 infection and other airborne diseases for surgical teams and patients. Some of the identified flaws were:
-Inadequate Airflow Direction: Traditional ventilation systems in operating theaters are primarily designed to create an airflow pattern that pushes air away from the operating table, aiming to reduce contamination in the sterile surgical zone. However, the study found that this airflow direction may not effectively mitigate the spread of aerosolized particles. Instead of directing contaminated air away from the surgical team, the airflow may circulate within the room, potentially exposing the surgical team to pathogens released by the patient or generated during surgical procedures.
-Circulation of Aerosolized Particles: One of the significant flaws identified is the circulation of aerosolized particles within the operating room. This circulation occurs due to the airflow patterns created by traditional ventilation systems, which can spread pathogens, including those carrying infectious diseases like COVID-19, throughout the room. Powered surgical tools, such as those used in minimally invasive procedures, can further contribute to the generation of aerosols, exacerbating the risk of airborne transmission.
-Exposure of Surgical Team: Despite the common practice of positioning support staff away from the patient and towards the operating room walls, the study found that these staff members are still at risk of exposure to airborne pathogens. The unintended circulation of aerosolized particles within the operating room puts the entire surgical team, including surgeons, nurses, anesthetists, and other operators, at a higher risk of infection. This contradicts the fundamental goal of protecting both patients and healthcare personnel from airborne contamination during surgical procedures.
-Impact on Surgical Safety: The flaws in existing ventilation systems pose significant challenges to surgical safety, particularly during the COVID-19 pandemic. With millions of elective surgeries being canceled or postponed worldwide due to safety concerns, addressing these flaws becomes imperative to ensure the continuity of essential medical care. The risk of airborne transmission in operating rooms underscores the need for innovative solutions to optimize ventilation systems and enhance healthcare safety protocols.
Overall, the study highlights the critical shortcomings of traditional ventilation systems in operating theaters, emphasizing the urgent need for a paradigm shift in ventilation system design. By addressing these flaws and implementing flexible, adaptable ventilation frameworks, healthcare facilities can significantly reduce the risk of airborne transmission of infectious agents, safeguarding the health and well-being of both patients and surgical teams.
Proposed Ventilation Framework
The researchers proposed a new, flexible ventilation framework that addresses the limitations of current systems. Through a combination of numerical modeling and experimental validation, the team identified key parameters influencing airflow patterns and particle circulation in different operating theater configurations. The optimized framework, named Configuration C3, features a single square inlet duct located on the ceiling above the patient area and four rectangular outlet ducts in the corners of the room. This modular design allows for different operation modes based on specific surgical needs, such as the presence of "surgical smoke" during procedures.
Implications for Healthcare Safety
The implications of this research are substantial for healthcare safety protocols, promising to revolutionize operating room practices and reduce the risk of airborne transmission in high-risk environments. By improving airflow dynamics, the proposed ventilation framework offers simple solutions for safer surgeries and better outcomes. Qasaimeh emphasized the significance of the research, stating that it equips the healthcare system to more effectively handle future outbreaks, ensuring the safety of both patients and clinical staff.
Discussion on Ventilation System Design and Evolution
The study delves into the historical evolution of ventilation systems in operating rooms, dating back to 1946 when the "air flow piston effect" was introduced. Over the years, the primary focus has been on protecting patients from airborne contaminants produced by the surgical team. However, the rise of powered surgical tools and the increased awareness of viral transmission through surgical aerosols have challenged the effectiveness of traditional ventilation systems. The study highlights the need for a paradigm shift in ventilation system design, considering the risk posed to the surgical team during procedures involving infectious diseases.
Challenges and Limitations
While the proposed ventilation framework shows promise in minimizing particle circulation, the study acknowledges certain limitations. The theoretical framework lacks routine surgical activity, and variations in surgical team dynamics and positions during procedures are not fully considered. The study suggests future research combining computer simulation studies with experiments to evaluate particle concentration, paving the way for the design and implementation of safer and more enhanced operating rooms.
Conclusion and Future Implications
The research conducted by NYUAD engineers serves as a groundbreaking exploration into the vulnerabilities of traditional ventilation systems in surgical operating theaters. The proposed ventilation framework provides a modular and adaptable solution to minimize airborne contamination, offering a crucial advancement in healthcare safety. The study's findings have far-reaching implications for future pandemics and the development of guidelines to ensure the safety of both patients and healthcare personnel. As the healthcare industry continues to evolve, optimizing ventilation systems in operating rooms becomes imperative to protect against airborne transmission of infectious agents and enhance overall patient and staff safety.
The study findings were published in the peer reviewed: journal: Life.
https://www.mdpi.com/2075-1729/14/3/313
For the latest
COVID-19 News, keep on logging to Thailand Medical News.