Researchers Warn That SARS-CoV-2 Is Triggering Neurodegenerative Diseases Like Parkinsons
Nikhil Prasad Fact checked by:Thailand Medical News Team Apr 11, 2024 1 year, 2 days, 5 hours, 8 minutes ago
COVID-19 News: The ongoing COVID-19 pandemic has not only challenged healthcare systems globally but has also raised concerns about its long-term impact on various bodily systems, including the nervous system. Researchers at the Indian Institute of Science Education and Research (IISER), Pune, India, have been closely studying the neurological consequences of COVID-19, particularly focusing on the potential link between SARS-CoV-2 infection and neurodegenerative diseases like Parkinson's disease (PD). In this
COVID-19 News report, we delve into the historical context of neurological complications following viral pandemics, the current understanding of neurological complications in COVID-19 patients, the conflicting evidence regarding the neurotropism of SARS-CoV-2, and the emerging connection between olfactory dysfunctions observed in long COVID and PD.
 SARS-CoV-2 Is Triggering Neurodegenerative Diseases Like Parkinsons
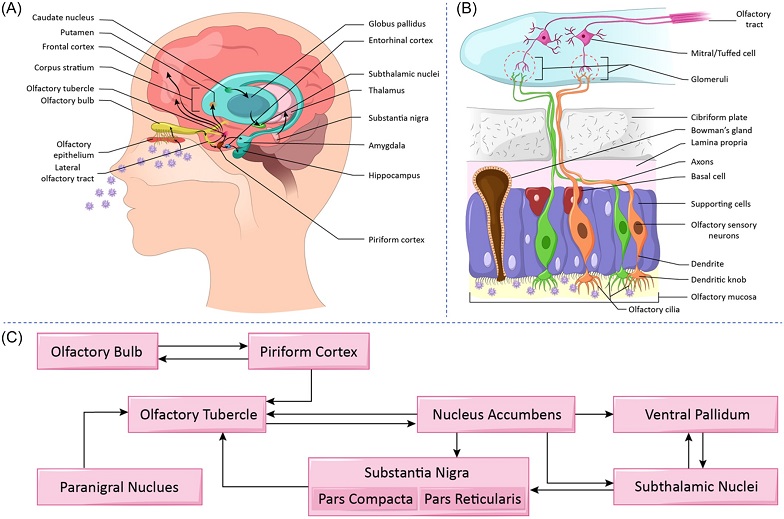
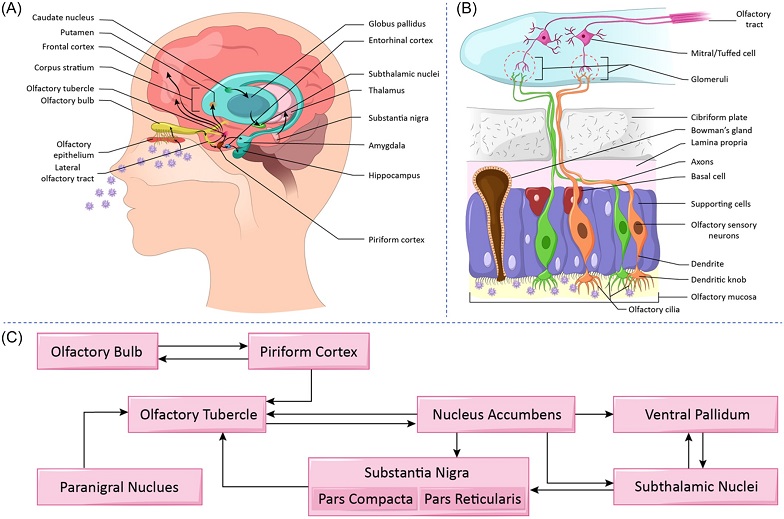
Understanding potential pathways underlying long-term pathological consequences of coronavirus disease 2019 (COVID-19) and incidence of Parkinson's Disease. (A) Schematic representation of potential transneuronal viral transmission routes. This depicts anatomical connections of olfactory cortical centers with mesocorticolimbic and nigro-striatal dopaminergic pathways involved in Parkinson's Disease pathology. (B) Schematic representation of olfactory pathway as a potential route for the central nervous system (CNS) invasion of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Olfactory system is highly vulnerable to external infectious agents due to its anatomical position. Bowman's gland secretion forms the mucosal lining of the olfactory epithelium, wherein viral particles get captured and largely infiltrate supporting cells, eventually affecting adjacent olfactory sensory neurons. The continuous connectivity between olfactory sensory neurons with M/T cells of the olfactory bulb could facilitate CNS invasion and transmission of the virus to different parts of the brain. (C) The diverse connectivity of olfactory cortical centers, i.e., piriform cortex and olfactory tubercle, with that of substantia nigra, subthalamic nucleus, and striatum that are involved in Parkinson's disease pathology.
Thailand Medical
SARS-CoV-2 Is Triggering Neurodegenerative Diseases Like Parkinsons
Understanding potential pathways underlying long-term pathological consequences of coronavirus disease 2019 (COVID-19) and incidence of Parkinson's Disease. (A) Schematic representation of potential transneuronal viral transmission routes. This depicts anatomical connections of olfactory cortical centers with mesocorticolimbic and nigro-striatal dopaminergic pathways involved in Parkinson's Disease pathology. (B) Schematic representation of olfactory pathway as a potential route for the central nervous system (CNS) invasion of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Olfactory system is highly vulnerable to external infectious agents due to its anatomical position. Bowman's gland secretion forms the mucosal lining of the olfactory epithelium, wherein viral particles get captured and largely infiltrate supporting cells, eventually affecting adjacent olfactory sensory neurons. The continuous connectivity between olfactory sensory neurons with M/T cells of the olfactory bulb could facilitate CNS invasion and transmission of the virus to different parts of the brain. (C) The diverse connectivity of olfactory cortical centers, i.e., piriform cortex and olfactory tubercle, with that of substantia nigra, subthalamic nucleus, and striatum that are involved in Parkinson's disease pathology.
Thailand Medical News had previously covered studies that also showed that SARS-CoV-2 infections can also lead to the development of various neurodegenerative diseases including Parkinson’s Disease.
https://www.thailandmedical.news/news/must-read-covid-19-effects-study-says-that-covid-19-could-lead-to-increase-in-parkinson-s-disease-among-those-infected
cases-emerging-showing-that-covid-19-infection-could-lead-to-parkinson-s-disease">https://www.thailandmedical.news/news/breaking-virus-news-documented-cases-emerging-showing-that-covid-19-infection-could-lead-to-parkinson-s-disease
https://www.thailandmedical.news/news/read-study-shows-sars-cov-2-n-protein-interacts-with-host-s-synuclein-proteins,-promoting-accelerated-amyloid-formation-and-parkinson-s-disease
https://www.thailandmedical.news/news/two-new-studies-shows-sars-cov-2-infections-will-ultimately-lead-to-enhanced-risk-of-developing-neurodegenerative-diseases-like-alzheimer-s-or-parkins
https://www.thailandmedical.news/news/university-of-oklahoma-study-discovers-how-the-polypeptide-sk9-from-the-envelope-protein-of-sars-cov-2-causes-parkinson-s-disease
https://www.thailandmedical.news/news/another-study-findings-adds-to-the-increasing-evidence-that-sars-cov-2-infection-increases-risk-of-brain-degeneration-that-will-lead-to-parkinson-s-di
https://www.thailandmedical.news/news/breaking-covid-19-news-italian-study-shows-that-sars-cov-2-infects-dopaminergic-neurons-and-hampers-dopamine-production
https://www.thailandmedical.news/news/covid-19-news-chronic-neuroinflammation-and-the-enigma-of-brain-fade-syndrome-in-neurological-diseases
https://www.thailandmedical.news/news/ferroptosis-possibly-behind-covid-19-induced-parkinson-s-disease-neurological-manifestations
Historical Perspective - Neurological Complications Following Viral Pandemics The history of viral epidemics and pandemics has been marked by various neurological complications, providing valuable insights into the potential long-term effects of COVID-19 on the nervous system. For instance, the emergence of encephalitis lethargica (EL) following the Spanish Influenza pandemic highlighted the neurological sequelae that can follow viral infections. EL, characterized by symptoms such as somnolence, hyperkinetic movements, and akinetic states, showed similarities with Parkinson's-like symptoms, raising concerns about a potential correlation between viral pandemics and the upsurge in neurological disorders.
Neurological Complications in COVID-19 Patients
As the COVID-19 pandemic progressed, reports of neurological complications among infected individuals began to surface. These complications ranged from mild symptoms such as anosmia and ageusia to more severe manifestations including encephalitis and long-lasting cognitive impairments. Studies conducted during the early phases of the pandemic indicated that a significant proportion of COVID-19 patients exhibited neurological symptoms, highlighting the need for comprehensive neurological assessments in both acute and post-acute phases of the infection.
Neurotropism of SARS-CoV-2
Conflicting Evidence One of the key areas of debate has been the neurotropism of SARS-CoV-2, i.e., its ability to infect and affect the central nervous system (CNS). While some studies have reported the presence of viral particles and proteins in various regions of the brain, others have questioned the direct neural invasion of the virus. The entry routes of the virus into the CNS, including the olfactory, ocular, and hematogenous pathways, have been explored, with emerging evidence suggesting potential neuroinvasive mechanisms involving both neuronal and non-neuronal cells.
Virus-Induced Neurodegeneration - Focus on Parkinson's Disease
Emerging evidence suggests a potential link between viral infections and the development or exacerbation of neurodegenerative diseases like Parkinson's Disease (PD). While the exact mechanisms remain elusive, several hypotheses shed light on how viruses might contribute to neurodegeneration, particularly in the context of PD.
Viral Triggers and Neuroinflammation
Viruses can act as triggers for neuroinflammation, initiating a cascade of immune responses that may lead to neuronal damage and dysfunction. In the case of PD, chronic neuroinflammation is believed to play a pivotal role in disease progression. Viral infections, especially those that persist or reactivate periodically, can sustain an inflammatory milieu in the brain, potentially accelerating neurodegenerative processes.
Molecular Mimicry and Autoimmunity
Another proposed mechanism is molecular mimicry, wherein viral proteins bear resemblance to host proteins involved in maintaining neuronal integrity. This similarity can lead to autoimmune reactions, where the immune system mistakenly targets both viral and host tissues, including dopaminergic neurons in the substantia nigra -the region primarily affected in PD. Autoimmune responses triggered by viral infections may contribute to the selective vulnerability of dopaminergic neurons observed in PD.
Neurotropic Viruses and CNS Invasion
Certain viruses exhibit neurotropism, meaning they have an affinity for neural tissues and can traverse the blood-brain barrier (BBB) to infect the central nervous system (CNS). Once inside the CNS, these viruses can directly interact with neurons and glial cells, causing neuronal dysfunction, synaptic alterations, and neurodegeneration. Herpesviruses, such as herpes simplex virus (HSV) and varicella-zoster virus (VZV), are known neurotropic viruses that have been implicated in CNS disorders, including potential associations with PD pathogenesis.
Viral-Induced Protein Aggregation
Some viruses can induce abnormal protein aggregation within neurons, a hallmark feature of many neurodegenerative diseases, including PD. For instance, viral proteins or viral-induced cellular stress responses may promote the misfolding and aggregation of alpha-synuclein, a key protein implicated in PD pathology. These aggregated proteins can disrupt cellular functions, impair neuronal viability, and contribute to the progressive nature of neurodegeneration.
Implications for Parkinson's Disease Research
Understanding the potential role of viral infections in PD pathogenesis has significant implications for disease research and therapeutic strategies. It prompts investigations into the interplay between viral factors, neuroinflammation, protein aggregation, and neuronal vulnerability in PD onset and progression.
Moreover, insights from virus-induced neurodegeneration may inform the development of novel therapies targeting immune modulation, viral clearance, or neuroprotective mechanisms to mitigate PD-related neurodegeneration.
Disease Olfactory dysfunctions, such as anosmia, hyposmia, and parosmia, have been observed as prevalent symptoms in both long COVID and PD. The olfactory system's vulnerability to viral infections and its role as a potential gateway for neurodegeneration have been explored. Emerging evidence suggests that persistent olfactory deficits in long COVID patients could indicate long-term damage to the olfactory system and potential implications for neurodegenerative diseases.
Conclusion
In conclusion, Indian researchers from IISER Pune have highlighted the potential link between SARS-CoV-2 infection and neurodegenerative diseases like Parkinson's disease, with a focus on olfactory dysfunctions as a common thread between long COVID and PD. While the exact mechanisms underlying this association require further elucidation, the historical context, clinical observations, and experimental evidence point towards a complex interplay between viral infections, neurological complications, and neurodegeneration. Continued research efforts, including long-term studies and animal models, are essential to unraveling the intricate pathways involved and developing targeted interventions for mitigating neurological sequelae of COVID-19. Elucidating these mechanisms holds promise for advancing our understanding of PD pathophysiology and paving the way for innovative therapeutic interventions aimed at halting or slowing disease progression.
The study findings were published in the peer reviewed journal: World Journal of Otorhinolaryngology - Head and Neck Surgery (Wiley).
https://onlinelibrary.wiley.com/doi/10.1002/wjo2.175
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/long-covid-19-news-one-in-three-infected-with-sars-cov-2-will-experience-neurological-or-psychiatric-issues-months-later-many-will-get-strokes
https://www.thailandmedical.news/news/study-uncovers-that-sars-cov-2-n-proteins-are-able-to-enter-stress-granules-and-cause-amyloid-aggregation,-leading-to-various-neurodegenerative-issues