Source: Brigham and Women's Hospital Jan 30, 2019 6 years, 2 months, 5 days, 1 hour, 43 minutes ago
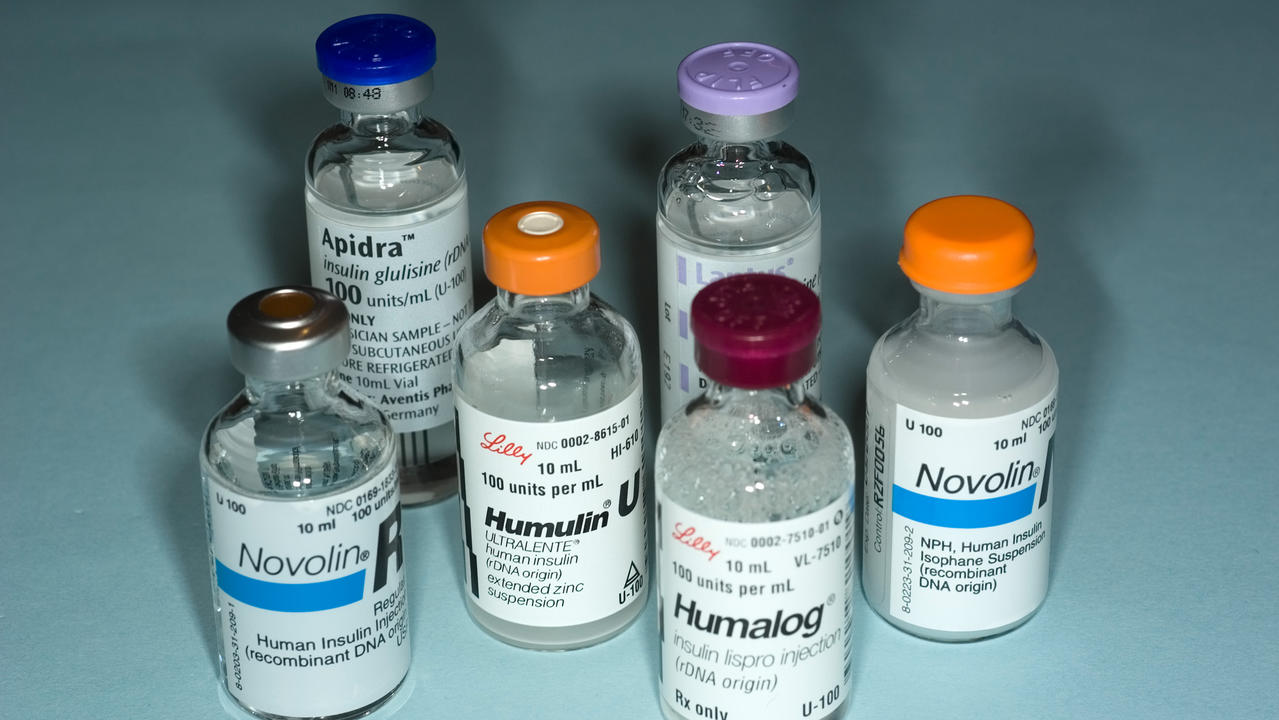
In the United States, the drug price for insulin has skyrocketed over the last two decades. While the price has increased for all forms of insulin, newer, "analogue" insulin medications such as glargine and lispro have become especially expensive.
This is particularly true for patients with insufficient drug coverage or for Medicare beneficiaries in the Part D coverage gap. CareMore Health, an integrated health delivery system and subsidiary of Anthem Inc., piloted an intervention to switch members from analogue to less expensive human insulin. Investigators from Brigham and Women's Hospital have analyzed the results of the program, finding that the switch was associated with only a small, population-level increase—0.14 percent—in hemoglobin A1c, a value that falls within expected biological variation. The findings appear in
The Journal of the American Medical Association.
"The change that we found is so small that I do not believe this is clinically meaningful or relevant," said corresponding author Jing Luo, MD, MPH, of the Program On Regulation, Therapeutics, And Law (PORTAL) in the Division of Pharmacoepidemiology and Pharmacoeconomics in the Department of Medicine at the Brigham. Luo also serves as a physician at the Phyllis Jen Center for Primary Care at the Brigham. "Importantly, we also found that this switch was not associated with serious hypoglycemic or hyperglycemic events and improved economic outcomes for patients and across the health system."
Luo and colleagues conducted a retrospective cohort study of 14,635 older adults with type 2 diabetes from four U.S. states (California, Arizona, Nevada and Virginia) participating in a Medicare Advantage plan. The team also compared results and outcomes for 983 participants who switched from analogue to human insulin to a comparative group of participants who did not switch. The primary outcome for the analysis was change in hemoglobin A1c levels before, during, and one year after the
health-plan-based intervention of switching patients from analogue to human insulin. Secondary outcomes included rates of serious hypoglycemia or hyperglycemia.
The research team found that before the intervention, mean hemoglobin A1c levels were 8.46 percent (an HbA1c of 7 to 8 percent is recommended by the American College of Physicians for most adults with type 2 diabetes) and decreased at a rate of 0.02 percent per month. When the intervention began, hemoglobin A1c levels increased by 0.14 percent. A year after the intervention was implemented, there were no significant differences in changes in hemoglobin a1c levels, neither in the entire population, nor in a subgroup of participants who made the switch.
In addition, the team analyzed rates of serious clinical adverse events related to changes in blood sugar. They found no significant differences in rates of serious events of either hypoglycemia or hyperglycemia when patients switched medications.
The team also analyzed economic outcomes, reporting that before the intervention, 89 percent of filled insulin prescriptions were for analogue insulin products. By December 2016, 70 percent of insulin prescriptions were for human insulin products. In 2014, 109 of 529 members (20.6 percent)
reached the Part D coverage gap. By 2016, this percent had dropped to 11.1 percent (143 of 1,289 members).
"The results of the current study add to a growing body of literature suggesting that human insulins may result in similar clinical outcomes compared with insulin analogues for many patients with
type 2 diabetes," said Luo in an interview with Thailand Medical News.
"Our study provides real-world evidence from clinical practice that should reassure patients, providers, and payors that it may be possible to switch to an older less expensive insulin to bring down costs while preserving quality of care."