SARS-CoV-2 Causes Phenotypic Alterations Of Circulating Follicular Helper T Cells In Severe COVID-19!
Nikhil Prasad Fact checked by:Thailand Medical News Team May 30, 2024 10 months, 3 weeks, 6 days, 10 hours, 47 minutes ago
COVID-19 News: The COVID-19 pandemic has provided researchers with a unique opportunity to study the immune system's response to a novel virus. One area of focus has been the behavior of circulating follicular helper T cells (cTfh), which are crucial for aiding B cells in producing high-affinity antibodies. This
COVID-19 News article delves into a study by researchers from University College London-United Kingdom and University of Tartu-Estonia that explores how severe COVID-19 influences the phenotype of cTfh cells and the subsequent impact on antibody responses.
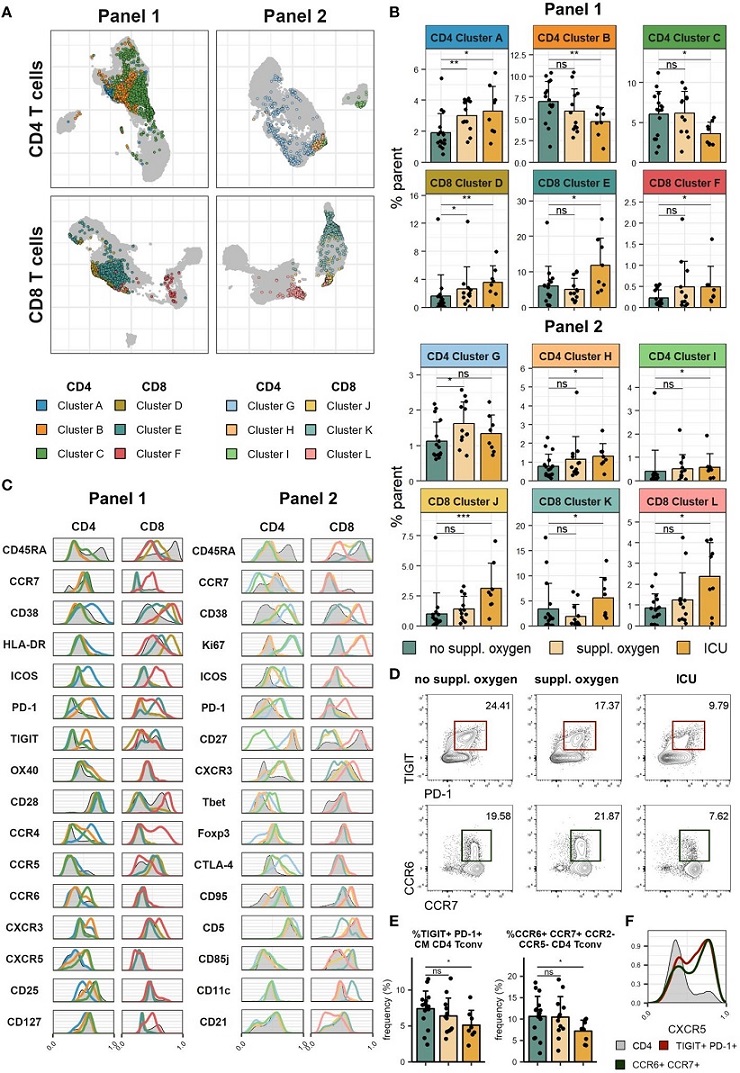
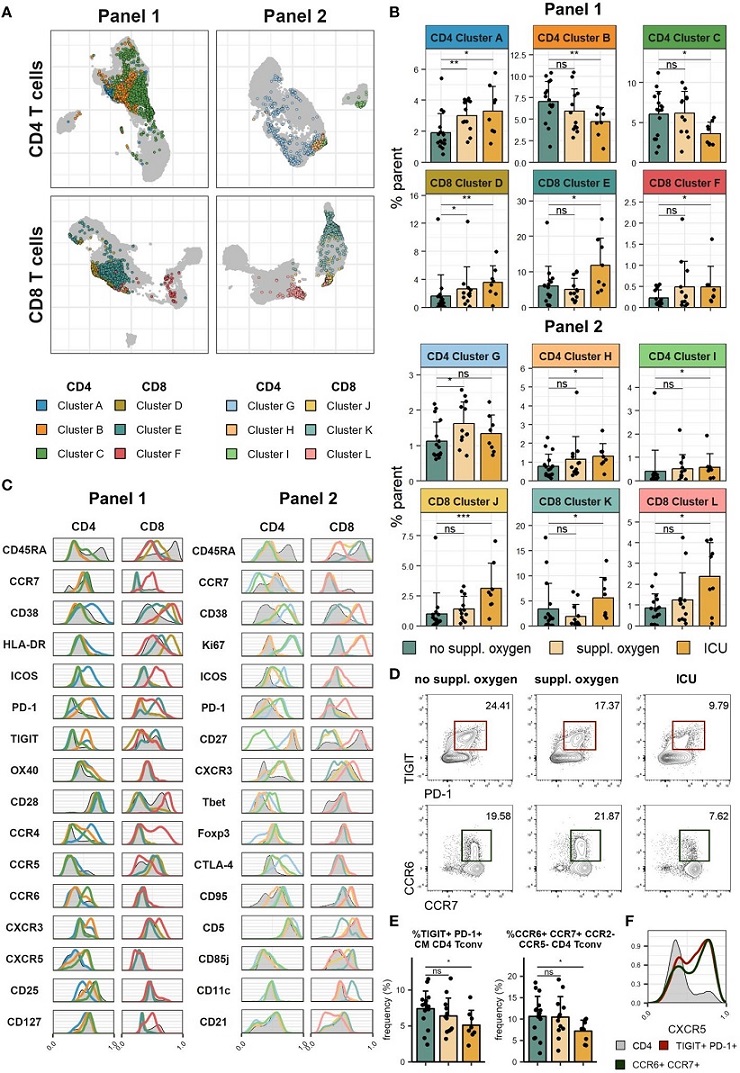 Severe COVID-19 is associated with increased T cell activation and proliferation. Cryopreserved PBMCs of individuals hospitalized with COVID-19 were analyzed using two spectral flow cytometry panels. (A) UMAP of CD4 (top) and CD8 (bottom) T cells in Panel 1 (left) and Panel 2 (right). Highlighted clusters are significantly different in frequency in disease severity groups. (B) Frequencies of clusters within CD4 and CD8 T cells of Panel 1 (top) and Panel 2 (bottom) significantly different between disease severity groups. (C) Histograms of marker expression of CD4 and CD8 T cell clusters (colour) and all CD4 and CD8 T cells (grey) in Panel 1 (left) and Panel 2 (right). (D) Representative flow cytometry plots of TIGIT+PD-1+ CM CD4 Tconv (top) and CCR6+CCR7+CCR2-CCR5- CD4 Tconv (bottom). (E) Frequency of TIGIT+PD-1+ CM CD4 Tconv (left) and CCR6+CCR7+CCR2-CCR5- CD4 Tconv (right) in disease severity groups. (F) Representative histograms of CXCR5 expression of TIGIT+PD-1+ CM CD4 Tconv (red), CCR6+CCR7+CCR2-CCR5- CD4 Tconv (green) and all CD4 T cells (grey). In (B, E) means + SD are shown. No suppl. oxygen, n = 16; Suppl. oxygen, n = 12; ICU, n = 8. Kruskal-Wallis (Cluster A, p = 0.008; Cluster B, p = 0.051; Cluster C, p = 0.060; Cluster D, p = 0.010; Cluster E, p = 0.050; Cluster F, p = 0.131; Cluster G, p = 0.069; Cluster H, p = 0.110; Cluster I, p = 0.080; Cluster J, p = 0.003; Cluster K, p = 0.034; Cluster L, p = 0.116; TIGIT+PD-1+ CM CD4 Tconv, p = 0.080; CCR6+CCR7+CCR2-CCR5- CD4 Tconv, p = 0.084) followed by two-tailed Mann–Whitney U-test; ***p < 0.001; **p < 0.01; *p < 0.05; ns, not significant.
The Role of Follicular Helper T Cells
Severe COVID-19 is associated with increased T cell activation and proliferation. Cryopreserved PBMCs of individuals hospitalized with COVID-19 were analyzed using two spectral flow cytometry panels. (A) UMAP of CD4 (top) and CD8 (bottom) T cells in Panel 1 (left) and Panel 2 (right). Highlighted clusters are significantly different in frequency in disease severity groups. (B) Frequencies of clusters within CD4 and CD8 T cells of Panel 1 (top) and Panel 2 (bottom) significantly different between disease severity groups. (C) Histograms of marker expression of CD4 and CD8 T cell clusters (colour) and all CD4 and CD8 T cells (grey) in Panel 1 (left) and Panel 2 (right). (D) Representative flow cytometry plots of TIGIT+PD-1+ CM CD4 Tconv (top) and CCR6+CCR7+CCR2-CCR5- CD4 Tconv (bottom). (E) Frequency of TIGIT+PD-1+ CM CD4 Tconv (left) and CCR6+CCR7+CCR2-CCR5- CD4 Tconv (right) in disease severity groups. (F) Representative histograms of CXCR5 expression of TIGIT+PD-1+ CM CD4 Tconv (red), CCR6+CCR7+CCR2-CCR5- CD4 Tconv (green) and all CD4 T cells (grey). In (B, E) means + SD are shown. No suppl. oxygen, n = 16; Suppl. oxygen, n = 12; ICU, n = 8. Kruskal-Wallis (Cluster A, p = 0.008; Cluster B, p = 0.051; Cluster C, p = 0.060; Cluster D, p = 0.010; Cluster E, p = 0.050; Cluster F, p = 0.131; Cluster G, p = 0.069; Cluster H, p = 0.110; Cluster I, p = 0.080; Cluster J, p = 0.003; Cluster K, p = 0.034; Cluster L, p = 0.116; TIGIT+PD-1+ CM CD4 Tconv, p = 0.080; CCR6+CCR7+CCR2-CCR5- CD4 Tconv, p = 0.084) followed by two-tailed Mann–Whitney U-test; ***p < 0.001; **p < 0.01; *p < 0.05; ns, not significant.
The Role of Follicular Helper T Cells
Follicular helper T cells (Tfh) play a critical role in the immune system by assisting B cells in the production of antibodies during germinal center reactions. While Tfh cells are typically found in secondary lymphoid organs, their blood-borne counterparts, cTfh, can be indicative of immune system status and are increasingly studied for their potential as biomarkers.
Immune Dysregulation in Severe COVID-19
Severe COVID-19 cases provide a paradigm for studying immune dysregulation. Researchers from University College London and the University of Tartu have examined the relationship between cTfh phenotype and antibody responses in patients with severe COVID-19. They found that severe disease was associated with higher levels of neutral
izing S1 IgG antibodies and increased T cell activation.
Activation Markers and TIGIT Expression
The study observed that cTfh cells expressing activation markers such as ICOS, CD38, and HLA-DR correlated positively with serum S1 IgG titres and neutralizing strength. Interestingly, the expression of the coinhibitory receptor TIGIT on cTfh cells was negatively correlated with these antibody responses. TIGIT+ cTfh cells showed increased levels of IFNγ and decreased levels of IL-17 compared to TIGIT- cTfh cells and demonstrated reduced capacity to help B cells in vitro.
Detailed Findings
-Severe COVID-19 and T Cell Phenotypes
The study utilized cryopreserved peripheral blood mononuclear cell (PBMC) samples from individuals hospitalized with COVID-19. Detailed immunophenotyping revealed distinct T cell phenotypes associated with severe disease, including increased expression of activation markers and proliferation markers like Ki67. These findings underscore the heightened immune activation in severe COVID-19 cases.
-TIGIT and B Cell Helper Function
One of the key findings was the reduced B-helper function of TIGIT+ cTfh cells. These cells expressed lower levels of CD40L, a molecule crucial for B cell activation. This reduced expression could explain the diminished capacity of TIGIT+ cTfh cells to aid B cells in producing antibodies.
-Cytokine Profiles
The cytokine profiles of TIGIT+ and TIGIT- cTfh cells also differed significantly. TIGIT+ cTfh cells produced more IFNγ, while TIGIT- cTfh cells produced higher levels of IL-17 and IL-21, which are important for B cell differentiation and survival. This cytokine skewing aligns with the functional differences observed between these cell subsets.
Implications for Disease Severity and Immune Response
-Antibody Responses and Disease Severity
The study found that higher titres of S1 IgG and stronger neutralizing antibodies were associated with severe COVID-19. This suggests that while a robust antibody response is generally protective, in the context of severe disease, it may also indicate a dysregulated or overactive immune response.
Potential Biomarkers
The differential expression of markers on cTfh cells in severe COVID-19 cases suggests that these cells could serve as biomarkers for disease severity. Specifically, the ratio of TIGIT+ to ICOS+CD38+ cTfh cells could be used to predict the strength of the antibody response and disease outcome.
Future Directions
-Understanding TIGIT+ cTfh Cells
Further research is needed to fully understand the role of TIGIT+ cTfh cells in the immune response. This includes exploring their interactions with other immune cells and their potential regulatory functions within germinal centers.
Clinical Applications
The findings highlight the potential of using cTfh cells as biomarkers in clinical settings. Monitoring the phenotypic changes in these cells could provide valuable insights into patient prognosis and the effectiveness of interventions such as vaccines.
Conclusion
The study by University College London and the University of Tartu provides significant insights into the phenotypic alterations of cTfh cells in severe COVID-19. The identification of TIGIT as a marker of cTfh cells with reduced B-helper function opens new avenues for research and potential clinical applications. As we continue to combat COVID-19 and future pandemics, understanding the nuances of the immune response will be crucial in developing effective treatments and vaccines.
In summary, this research underscores the complex interplay between the immune system and SARS-CoV-2, highlighting the importance of cTfh cells in shaping the body's defense mechanisms. The findings not only advance our knowledge of COVID-19 pathogenesis but also pave the way for innovative approaches to immune monitoring and therapy.
The study findings were published in the peer reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1395684/full
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/why-your-immune-system-doesn-t-remember-covid-19-well-new-findings-on-cd4-t-cells
https://www.thailandmedical.news/news/influence-of-cross-reactive-t-cells-in-sars-cov-2-infections
https://www.thailandmedical.news/news/persistent-t-cell-dependent-ifn-gamma-release-seen-in-long-covid-individuals