SARS-CoV-2 Disrupts Eosinophils While COVID-19 Vaccines Cause Eosinophilia and Induce Immunopathogenicity!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 24, 2025 3 weeks, 1 day, 34 minutes ago
Medical News: In a new eye-opening study, researchers from Aix Marseille University and IHU-Méditerranée Infection in Marseille, France, in collaboration with scientists from the Laboratory of Immunology and INSERM UMR-S 1250 P3CELL at the University Hospital of Reims, have unveiled a worrying duality in how COVID-19 and its vaccines affect a lesser-known but crucial group of immune cells - eosinophils. Their findings paint a picture of immune confusion, potential vaccine complications, and the critical need for more tailored immunological approaches to SARS-CoV-2.
 SARS-CoV-2 Disrupts Eosinophils While COVID-19 Vaccines Cause Eosinophilia and
SARS-CoV-2 Disrupts Eosinophils While COVID-19 Vaccines Cause Eosinophilia and
Induce Immunopathogenicity
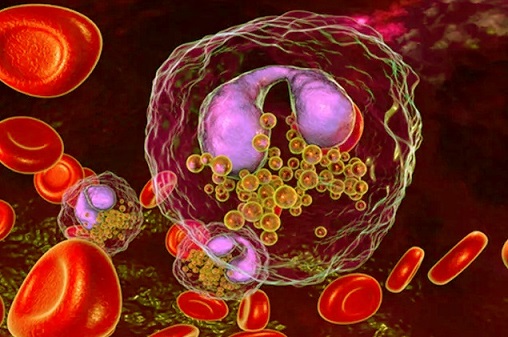
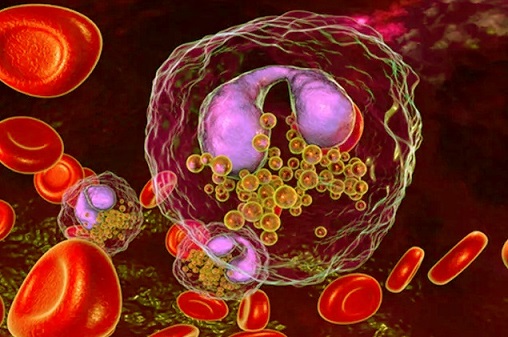
Eosinophils, long overshadowed by white blood cells like lymphocytes and neutrophils, have emerged as major players in COVID-19 pathology. While these cells are often known for their roles in allergies and asthma, their functions extend to fighting viruses, shaping immune responses, and maintaining tissue homeostasis. However, SARS-CoV-2 seems to have a disruptive grip on eosinophils, depleting their numbers and skewing their activity during infection.
In stark contrast, COVID-19 vaccines - especially those using adjuvants like aluminum or excipients such as polyethylene glycol (PEG) - may trigger excessive eosinophil activation, leading to dangerous inflammation in the lungs and other tissues. This
Medical News report dives deep into this paradoxical tale of disruption and overstimulation, raising questions about safety, vaccine design, and long-term outcomes for both infected and vaccinated individuals.
Eosinophils Disappear During Infection but Reappear with a Vengeance in Post-Vaccination
One of the earliest clinical signs observed in hospitalized COVID-19 patients is eosinopenia - a marked decrease in the number of eosinophils in the blood. This drop occurs across all severities of disease but is most severe in critically ill patients. According to the researchers, over 80% of COVID-19 fatalities reviewed had below-normal eosinophil levels at admission. This depletion isn't fully understood, but the scientists point to several plausible mechanisms.
SARS-CoV-2 may directly affect eosinophil production by disrupting bone marrow function or triggering apoptosis (programmed cell death). It may also infect eosinophils through a surface receptor known as basigin or CD147. Notably, eosinophils from COVID-19 patients show high expression of this receptor early in infection. This suggests that SARS-CoV-2 might exploit basigin for entry, as it does with platelets, which the virus has been shown to infect and destroy.
Furthermore, inflammatory cytokines such as IFN-γ, TNF-α, and Type I interferons - which are elevated during acute COVID-19 - can also drive eosinophil death or cause them to migrate aggressively into the lungs. Once there, they may either help fight the virus or exacerbate lung injury depending on the surrounding immune context.
When Eosinophils Become Double Agents
;
Despite their antiviral potential, eosinophils can paradoxically become drivers of inflammation and tissue damage. Their granular contents - particularly eosinophil cationic protein (ECP) and eosinophil-derived neurotoxin (EDN) - can degrade viral RNA but also stimulate a flood of cytokines, recruiting more inflammatory cells and igniting a dangerous immune cascade.
These same eosinophils also express PD-L1, a molecule that interacts with PD-1 on T-cells to suppress immune responses. This interaction may help explain the common finding of lymphopenia (low lymphocyte count) in COVID-19 patients. Essentially, eosinophils may be sabotaging the adaptive immune response by directly contributing to T-cell exhaustion or death.
In addition, the study uncovered evidence that high eosinophil activation - marked by the expression of CD69 and CD62L - is associated with lung injury severity and the need for mechanical oxygen support. This indicates that eosinophil migration and hyperactivation might be a precursor to acute respiratory distress syndrome (ARDS) in COVID-19 patients.
Asthma Patients Surprisingly Spared
Interestingly, people with asthma - particularly those with allergic, eosinophilic asthma - do not appear to be at higher risk of severe COVID-19. In fact, several studies suggest they may be protected. This is a surprising twist, considering asthma is typically viewed as a risk factor in other viral respiratory infections.
The researchers propose that asthma patients' immune environments, which are dominated by type 2 cytokines such as IL-4, IL-5, and IL-13, may actually blunt the cytokine storm seen in severe COVID-19. IL-13, in particular, can suppress inflammatory macrophage activity and promote healing by polarizing immune cells toward a less aggressive, tissue-repairing state.
Additionally, common asthma medications such as corticosteroids and biologics targeting IL-5 (like mepolizumab and benralizumab) may further temper eosinophil-driven inflammation. This could explain why eosinophilic asthma, paradoxically, may act as a shield rather than a liability during SARS-CoV-2 infection.
COVID-19 Vaccines Trigger Eosinophilic Overdrive
While natural SARS-CoV-2 infection leads to eosinophil depletion, the opposite seems to occur following COVID-19 vaccination. In numerous documented cases, vaccines - especially those containing adjuvants like aluminum (used in Sinovac/CoronaVac) or excipients like PEG and polysorbate 80 (used in Pfizer, Moderna, and AstraZeneca) - have caused serious eosinophil-mediated complications.
Reports include eosinophilic pneumonia, myocarditis, angioedema with eosinophilia, eosinophilic gastroenteritis, and even fatal systemic eosinophilic infiltration. In one alarming case, a 73-year-old woman developed pulmonary eosinophilia just seven weeks after receiving a Sinovac vaccine. Another case involved fatal eosinophilic myocarditis following Pfizer mRNA vaccination. A 64-year-old man developed a pustular skin eruption with heavy eosinophil infiltration only four days after a Pfizer jab.
Eosinophilic complications have also been found in children, including a 12-year-old boy who developed eosinophilic cellulitis. These findings point to a consistent pattern of post-vaccine eosinophil dysregulation, regardless of age, sex, or health history.
The Role of Vaccine Ingredients
The immunopathology seen after vaccination appears to be tightly linked to vaccine components. Aluminum-based adjuvants stimulate Th2 immune responses, which promote eosinophil maturation and tissue migration while reducing regulatory T-cell (Treg) function. PEG and tromethamine, found in many mRNA vaccines, are known to cause hypersensitivity reactions. These chemicals can activate the complement system, releasing potent inflammatory molecules (C3a and C5a) that attract eosinophils and worsen inflammation.
Even polysorbate 80, found in the AstraZeneca vaccine, may cross-react with PEG and trigger similar reactions. In some cases, anti-PEG antibodies are produced, not only reducing vaccine efficacy but also potentially provoking harmful eosinophilic responses.
Interestingly, mouse models of coronavirus vaccination showed that incorporating a Toll-like receptor agonist in the vaccine design helped prevent eosinophilic lung inflammation while still producing strong antibody responses. This finding suggests that vaccine formulations can be improved to avoid these dangerous outcomes.
The Bigger Picture
While eosinophils have long been overlooked in discussions of COVID-19 pathology and vaccine safety, this study puts them squarely in the spotlight. They appear to play a dual role - first as defenders against the virus, then as potential agents of collateral damage, especially in the lungs and cardiovascular system.
Understanding this duality is crucial as we move forward with ongoing vaccine campaigns, long COVID management, and new SARS-CoV-2 variants. Vaccine design must evolve to consider not only antibody response but also the inflammatory potential of immune cells like eosinophils. Excluding problematic adjuvants and excipients, or premedicating sensitive individuals with antihistamines or corticosteroids, could be viable strategies to prevent eosinophil-driven complications.
Conclusion
The findings of this study serve as a stark reminder that the immune system is not always our friend in the battle against SARS-CoV-2. While eosinophils can be powerful allies in viral clearance, their overactivation - especially after vaccination - may lead to severe organ damage and even death. This dual nature makes them both heroes and villains of the COVID-19 narrative. Their behavior during natural infection reveals a pattern of depletion and dysfunction, potentially driven by viral infection, cytokine storms, and disrupted bone marrow activity. In contrast, vaccination - though life-saving for millions - can inadvertently trigger eosinophilic overdrive, especially in those with sensitivities to vaccine components. This underscores the urgent need for safer vaccine formulations and individualized approaches to immunization. Monitoring eosinophil levels before and after vaccination could become a key step in identifying at-risk individuals. The path forward must balance immunogenicity with safety, particularly as new variants and booster strategies emerge. Ultimately, deeper understanding of eosinophils could offer new pathways not only for COVID-19 management but also for broader vaccine safety and immune system modulation.
The study findings were published in the peer-reviewed journal: Clinical and Translational Allergy.
https://onlinelibrary.wiley.com/doi/10.1002/clt2.70050
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/eosinophils-as-predictors-of-lung-complications-in-covid-19
https://www.thailandmedical.news/news/breaking-japanese-physicians-warns-that-even-asymptomatic-sars-cov-2-infections-can-trigger-acute-exacerbation-of-idiopathic-hypereosinophilic-syndrom
https://www.thailandmedical.news/news/must-read-covid-19-diagnostics-research-indicates-that-eosinophil-count-is-a-better-biomarker-for-covid-19-than-current-testing-platforms
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings
https://www.thailandmedical.news/articles/hospital-news
https://www.thailandmedical.news/pages/thailand_hospital_listings