SARS-CoV-2 Infections Literally Causes Your Brain Cells To Die! More Emerging Cases Of Post COVID Acute Necrotizing Encephalopathy In Young Adults!
COVID-19 News - SARS-CoV-2 - Acute Necrotizing Encephalopathy Apr 14, 2023 2 years, 4 days, 13 hours, 28 minutes ago
COVID-19 News: Once considered rare in the beginning of the COVID-19 pandemic, more cases studies of acute necrotizing encephalopathy are emerging globally with a new trend showing that its now mostly young adults or infants developing the condition!
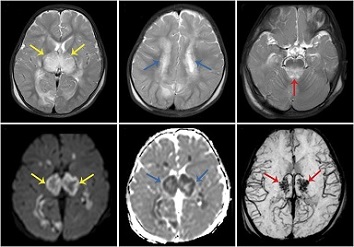
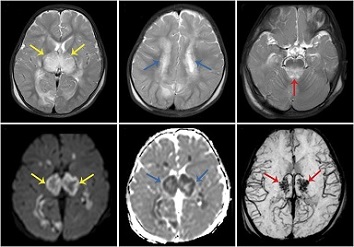
Acute necrotizing encephalopathy (ANE) was first described in 1995 as a complication of viral respiratory tract infection in pediatric patients, with RNA viruses implicated in most cases. It is characterized by the presence of symmetrical multifocal lesions with predominantly thalamic involvement, as well as the involvement of the brainstem, white matter of the brain, and cerebellum. On tomography images, the lesions are hypodense with respect to the gray matter, and MRI shows a hypointense signal in T1, hyperintense in T2, hyperintense in FLAIR with internal hemorrhage plus restriction of the regions involved and with ring enhancement after administration of gadolinium.
To date, there has been numerous case reports of acute necrotizing encephalopathy in post COVID individuals as reported in various studies or
COVID-19 News coverages.
https://www.thailandmedical.news/news/breaking-covid-19-news-china-reports-first-case-of-necrotizing-encephalopathy-in-infant-due-to-sars-cov-2-new-variants-changing-course
https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-022-07610-0
https://www.cureus.com/articles/87157-acute-necrotizing-encephalitis-as-an-early-manifestation-of-covid-19#!/
https://rescon.jssuni.edu.in/radiologyteachingfiles/2/
https://www.cureus.com/articles/53650-acute-necrotizing-encephalopathy-associated-with-sars-cov-2-exposure-in-a-pediatric-patient#!/
https://www.jpeds.com/article/S0022-3476(22)00346-8/fulltext
https://www.frontiersin.org/articles/10.3389/fneur.2022.872734/full
https://n.neurology.org/content/95/10/445
https://jnnp.bmj.com/content/91/9/1004
https://journals.sagepub.com/doi/full/10.1177/2050313X221083653
https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/en/covidwho-999777
https://pubs.rsna.org/doi/full/10.1148/radiol.2020201187
https://ejnpn.springeropen.com/articles/10.1186/s41983-021-00413-1
https://onlinelibrary.wiley.com/doi/10.1111/ene.14966
https://www.microbiologyresearch.org/content/journal/acmi/10.1099/acmi.0.000546.v2
https://www.ijidonline.com/article/S1201-9712(21)01232-7/fulltext
https://www.ejpn-journal.com/article/S1090-3798(23)00025-9/fulltext
https://journals.lww.com/neurotodayonline/blog/breakingnews/pages/post.aspx?PostID=926
In yet another new case study submitted by researchers from the National Institute of Neurology and Neurosurgery Manuel Velasco Suarez -Mexico, a young 26-year-old male adult was also diagnosed with Post COVID Acute Necrotizing Encephalopathy based on MRI findings.
The study team described the case of a 26-year-old male, with a medical history of medulloblastoma that was disease-free after treatment, and who tested positive in a PCR for SARS-CoV-2 in cerebrospinal fluid. Upon evaluation at the emergency department one week later, the patient was found to be awake, oriented, and focused, and could maintain attention for periods. Mixed dysarthria persisted, characterized by being flaccid and hypokinetic. On magnetic resonance imaging, there were multiple hemorrhagic lesions with surrounding edema in the right thalamus with an extension to the posterior arm of the internal capsule, a smaller one, in the left thalamus, and another expanded to the ipsilateral peduncle.
According to the study team, acute necrotizing encephalopathy presents a great clinical and diagnostic challenge, Close clinical and radiological follow-up is essential, and magnetic susceptibility sequences (T2 or SWI) should be included in the diagnosis protocol.
This new case report highlights the importance of considering neurological complications in patients with antecedent of COVID-19 infection, especially those with severe and atypical symptoms.
MRI or magnetic resonance imaging is considered the study of choice for SARS-CoV-2-related neurological damage. Characteristic imaging features include symmetrical multifocal lesions, predominantly in the thalamus, brainstem, brain white matter, and cerebellum. These lesions are hypodense on tomography images and hyperintense on T2/FLAIR, with areas of internal bleeding. Magnetic susceptibility sequences such as T2 or SWI, after administration with gadolinium, may show variable enhancement patterns, such as dotted, linear, annular, or incomplete annular. Although this is a single case in an adult patient, therefore cannot establish causality or generalizability.
The SARS-CoV-2 virus can cause neurological damage through various mechanisms, such as direct damage to specific receptors, cytokine-associated lesions, retrograde progression through nerve fibers, and secondary hypoxia. When SARS-CoV-2 binds to the pulmonary epithelium, a systemic inflammatory response involving interleukins such as IL-6, IL-12, IL-15, and TNF-a is generated, which activates glial cells and produces a massive pro-inflammatory state, leading to alterations in the nervous system.
Acute necrotizing encephalopathy after SARS-CoV-2 infection has been described in a growing number of cases recently cases and should not be neglected in the differential diagnosis of neurological complications in patients with radiological image alterations, as evidence suggests that patients recovered from a severe COVID-19 picture may present a cytokine storm syndrome, particularly interleukin-6.
It is also important to note that SARS-CoV-2-related neurological complications are not limited to the acute phase of the illness. Some studies have reported that patients who have recovered from COVID-19 may continue to experience neurological symptoms such as cognitive impairment, fatigue, and headaches for an extended period, which is referred to as post-acute sequelae of SARS-CoV-2 infection.
Acute necrotizing encephalopathy presents a great clinical and diagnostic challenge, close clinical and radiological follow-up is essential, and magnetic susceptibility sequences (T2 or SWI) should be included in the diagnosis protocol. Early recognition and intervention are key to preventing mortality and improving patient outcomes.
The study findings were published on a preprint server and are currently being for peer reviewed for publication in the journal: SN Comprehensive Clinical Medicine (Springer).
https://www.researchsquare.com/article/rs-2752907/v1
For the latest
COVID-19 News, keep on logging to Thailand Medical News.