SARS-CoV-2 ORF3A Protein Hijacks CLCC1 Chloride Channel to Cause Endoplasmic Reticulum Dysfunction
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 19, 2024 1 year, 2 weeks, 5 days, 7 hours, 34 minutes ago
Medical News: In an important breakthrough, a team of researchers from Tsinghua University and China CDC has uncovered a new mechanism behind the damage caused by SARS-CoV-2, the virus responsible for COVID-19. The scientists revealed that the virus’s ORF3A protein interacts with a vital cellular component, the CLCC1 chloride channel, leading to disruptions in the endoplasmic reticulum (ER). This dysfunction in ER plays a crucial role in cellular stress, organ damage, and even neurological symptoms seen in COVID-19 patients.
 SARS-CoV-2 ORF3A Protein Hijacks CLCC1 Chloride Channel to Cause Endoplasmic Reticulum Dysfunction
SARS-CoV-2 ORF3A Protein Hijacks CLCC1 Chloride Channel to Cause Endoplasmic Reticulum Dysfunction
The study highlights how the SARS-CoV-2 ORF3A protein hijacks the CLCC1 channel, causing ER stress and triggering severe cellular consequences. These findings could pave the way for potential therapeutic targets aimed at alleviating the damage caused by the virus.
The Hidden Role of ORF3A and CLCC1
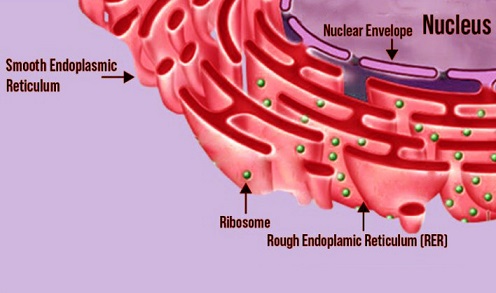
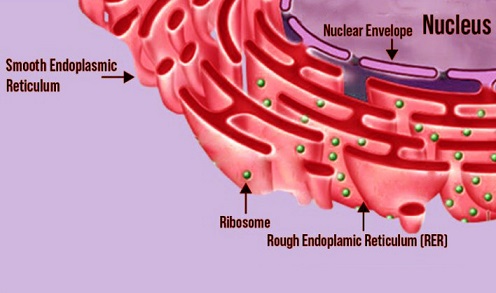
The endoplasmic reticulum, often referred to as the cell’s protein factory, is responsible for processing and folding proteins. It is also essential for maintaining cellular ion balance. However, SARS-CoV-2 appears to exploit this system to aid its infection and survival. Researchers discovered that the virus’s ORF3A protein directly interacts with CLCC1, an ER-resident chloride channel that regulates ion homeostasis within the ER.
CLCC1 plays a critical role in maintaining the correct concentrations of chloride (Cl⁻), potassium (K⁻), and calcium (Ca²⁻) ions inside the ER. Proper ion balance ensures smooth protein folding and prevents cellular stress. This
Medical News report dives deep into how ORF3A disrupts this balance and causes widespread cellular damage.
What the Researchers Found
The study, conducted by scientists at Tsinghua University, including Dr. Liang Guo, Baoying Huang, and Yichang Jia, and collaborators from China CDC, examined how ORF3A hijacks the CLCC1 channel. Using advanced molecular biology tools and live-cell imaging, the team demonstrated that ORF3A interaction with CLCC1 impairs the ER’s ionic environment. Specifically, the researchers found:
-Disrupted Ion Homeostasis: When ORF3A binds to CLCC1, it leads to abnormal ion levels inside the ER. The levels of chloride and potassium ions increase, while calcium levels drop significantly. These changes disrupt protein folding, a process essential for cell function and survival.
-Unfolded Protein Response (UPR): The ER’s failure to fold proteins properly activates the UPR, a stress response mechanism. The team observed increased markers of ER stress, such as the activation of IRE1, PERK, and ATF6 pathways. These pathways act as alarms, signaling that the ER is overwhelmed.
-ER Phagy and Nucleophagy: Under severe stress, the cell resorts to a survival mechanism called autophagy, where damaged cellular components are degraded
and recycled. The study found that ORF3A expression triggers ER-phagy (destruction of ER membranes) and nucleophagy (destruction of nuclear components). Newly developed ratiometric sensors confirmed these processes.
-Formation of CLCC1 Clusters: ORF3A induces the clustering of CLCC1 channels within the ER, particularly around the nucleus. These clusters disrupt normal ER functions, amplifying cellular damage.
Impact on Mouse Models and Human Cells
To further validate their findings, the researchers conducted experiments in mouse models. When ORF3A was introduced into the brains of mice, the results were alarming. The animals showed severe ER stress, protein misfolding, and apoptosis (cell death) in brain cells.
Electron microscopy revealed significant changes in ER morphology, including the formation of concentric whorls and membrane blebs. These findings correlate with neurological symptoms observed in COVID-19 patients, such as headaches, cognitive impairment, and even strokes.
Interestingly, the study showed that increasing the levels of CLCC1 in cells could partially reverse the toxic effects caused by ORF3A. By sequestering ORF3A within the ER, elevated CLCC1 levels reduced cellular stress and autophagy, offering hope for potential therapeutic interventions.
The Conservation of ORF3A Function
One of the most intriguing aspects of this study is that the damaging effects of ORF3A are not unique to SARS-CoV-2. The researchers tested ORF3A proteins from related coronaviruses, such as SARS-CoV-1, bat coronaviruses (BtCoV HKU3), and pangolin coronaviruses (PCoV GX-P5L). All these ORF3A proteins interacted with CLCC1 and triggered similar disruptions in ER function, suggesting a conserved mechanism across beta-coronaviruses.
This conservation indicates that the ORF3A-CLCC1 interaction is a fundamental viral strategy for hijacking host cells and causing damage. It also raises questions about whether animals carrying these coronaviruses experience similar cellular stress and how their systems might adapt to this viral interference.
Why This Matters
COVID-19 has impacted millions worldwide, with lingering health issues, including neurological symptoms, persisting in many recovered patients. By understanding how SARS-CoV-2 ORF3A disrupts CLCC1 and causes ER dysfunction, scientists now have a clearer picture of the virus’s pathology.
The study also opens new doors for therapeutic strategies. For instance, increasing CLCC1 expression in cells could serve as a targeted intervention to mitigate ORF3A-induced cellular damage. Therapies designed to stabilize ER ion balance or block the ORF3A-CLCC1 interaction could help alleviate severe COVID-19 symptoms.
Conclusion
The discovery that SARS-CoV-2 ORF3A protein hijacks the CLCC1 chloride channel to disrupt ER function provides critical insights into the virus’s pathogenesis. This interaction triggers ER stress, ion imbalances, and severe cellular damage, leading to symptoms that extend beyond the respiratory system and into the brain.
The findings highlight the importance of targeting viral accessory proteins like ORF3A in the development of therapies for COVID-19. By stabilizing CLCC1 functions or blocking its interaction with ORF3A, researchers could mitigate the long-term effects of the virus and improve patient outcomes. This study also underscores the need for continued research into conserved viral mechanisms, especially among beta-coronaviruses, which remain a global health threat.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.researchsquare.com/article/rs-5241039/v1
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/sars-cov-2-alters-host-cell-organelles-while-reshaping-cellular-processes-and-pathways
https://www.thailandmedical.news/news/university-of-california-study-finds-that-sars-cov-2-nsp4-protein-alters-endoplasmic-reticulum-structure
https://www.thailandmedical.news/news/new-insights-into-reticulophagy-and-its-role-in-viral-infections
https://www.thailandmedical.news/articles/coronavirus