Scientists from Chile Discover That Human Metapneumovirus Infections Also Affect Both Innate and Adaptive Intestinal Immunity
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 31, 2024 3 months, 3 weeks, 5 days, 3 hours, 33 minutes ago
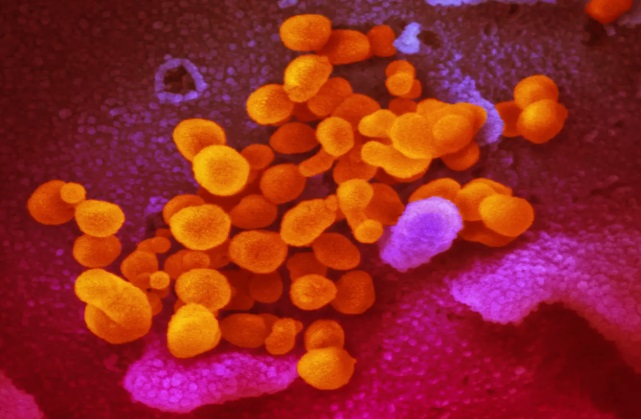
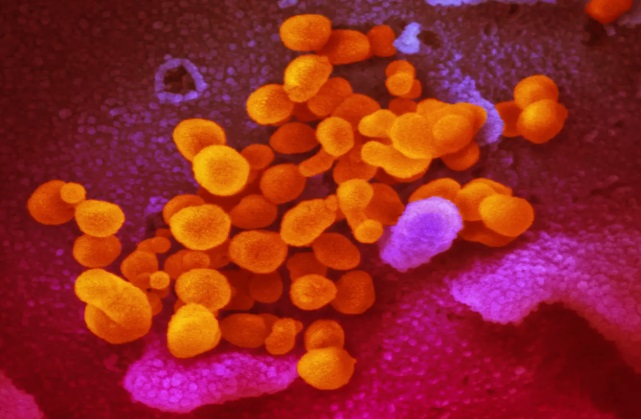
HMPV News: Human metapneumovirus (HMPV), a relatively under-explored respiratory virus, is drawing attention for its potential to influence not only lung health but also intestinal immunity. This development in medical research could transform our understanding of how respiratory infections extend their impact beyond the lungs. Researchers from Pontificia Universidad Católica de Chile and Universidad Andrés Bello have collaborated to explore this intriguing connection.
While HMPV primarily affects children under five and is a leading cause of infant mortality due to pneumonia, its effects on intestinal immunity have been largely overlooked. This
HMPV News report delves into recent findings from a mouse model study that sheds light on how respiratory viruses may indirectly influence gut health.
 Scientists from Chile Discover That Human Metapneumovirus Infections Also Affect Both
Scientists from Chile Discover That Human Metapneumovirus Infections Also Affect Both
and Adaptive Intestinal Immunity
Studying the Lung-Gut Axis
The study began by examining whether HMPV, which is known to cause pneumonia, affects the gut directly. Intranasal infections were conducted on mice, and samples were analyzed at various time points post-infection. Despite no detectable viral load in the intestine, significant immune changes were observed in the colon. For instance, at day one post-infection, there was a marked increase in the transcription of interferon-gamma (IFN-γ), a pro-inflammatory cytokine.
The researchers aimed to uncover whether these immune responses were linked to direct viral invasion or indirect effects such as systemic inflammation. Flow cytometry and molecular techniques revealed key alterations in both innate and adaptive immune responses in the gut.
Key Findings on Intestinal Immunity
-Innate Immune Response:
Monocyte populations showed notable fluctuations. Ly6C+ MHCII+ monocytes - a marker for inflammation - peaked early in the infection before subsiding by day five.
However, neutrophils and macrophages did not exhibit significant changes, suggesting a specific immune cell response to HMPV.
-Adaptive Immune Response:
CD8+ T cells, critical for adaptive immunity, showed an increased presence in the colon by day five. Interestingly, a subset of these cells, memory precursor effector CD8+ T cells, was also elevated, pointing to long-term immune modulation.
Despite these changes, IgA-producing plasma cells - key to gut microbiota regulation - remained unaffected, as did levels of IgA in fecal samples.
-Microbiota Stability:
The study used 16S rRNA sequencing to analyze changes in gut microbiota composition. While minor alterations were observed, they were not statistically significant. For example, the family Lactobacillaceae showed a transient decrease but returned to baseline by day five. Alpha and beta diversity measures confirmed
that the gut microbiota remained largely stable during the infection period.
Implications and Unanswered Questions
The study’s findings indicate that HMPV triggers temporary but targeted immune changes in the gut. Unlike other respiratory viruses, such as influenza, which can cause significant gut inflammation and microbiota disruption, HMPV appears to have a more restrained impact. This raises important questions about the mechanisms driving these changes. Could they be attributed to systemic inflammatory signals from the lungs, or might there be a yet-undiscovered pathway linking lung infections to gut immunity?
Moreover, the absence of significant microbiota changes suggests that HMPV’s effects may be immune-mediated rather than microbiota-dependent. This insight challenges prevailing theories about the lung-gut axis and emphasizes the need for further research.
Conclusions
The study underscores the complexity of the lung-gut axis and highlights how respiratory infections can ripple through the body’s immune systems. While HMPV does not directly invade the gut, it subtly influences gut immunity by modulating monocyte and CD8+ T cell populations. These findings pave the way for more nuanced research into how respiratory infections affect overall health.
By understanding these connections, we can better prepare for interventions that mitigate the broader impacts of respiratory illnesses. Future studies should explore whether these immune changes influence susceptibility to secondary gut infections or long-term intestinal health.
The study findings were published in the peer-reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1330209/full
For the latest HMPV News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/israeli-study-finds-that-human-metapneumovirus-uses-unique-strategy-to-escape-recognition-by-nk-cells
https://www.thailandmedical.news/news/louisiana-study-finds-that-human-metapneumovirus-uses-mirnas-to-impair-immune-responses-involving-interferons
https://www.thailandmedical.news/news/human-metapneumovirus-infections-on-the-rise-in-china
https://www.thailandmedical.news/articles/hmpv-human-metapneumovirus