Scientists from Singapore Discover Plasma Biomarkers That Identify Blood-Brain Barrier Dysregulation in Alzheimer’s Disease
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 04, 2024 6 months, 3 weeks, 20 hours, 48 minutes ago
Medical News: A group of scientists from Singapore has made an exciting discovery in Alzheimer’s disease research, identifying plasma biomarkers that can reveal blood-brain barrier (BBB) dysregulation, a key element in the progression of the disease. This breakthrough brings new hope for better diagnostics and treatments for Alzheimer’s, a condition that affects millions of people worldwide. This
Medical News report will delve into the fascinating details of their discovery and how it might change the landscape of Alzheimer's disease diagnosis.
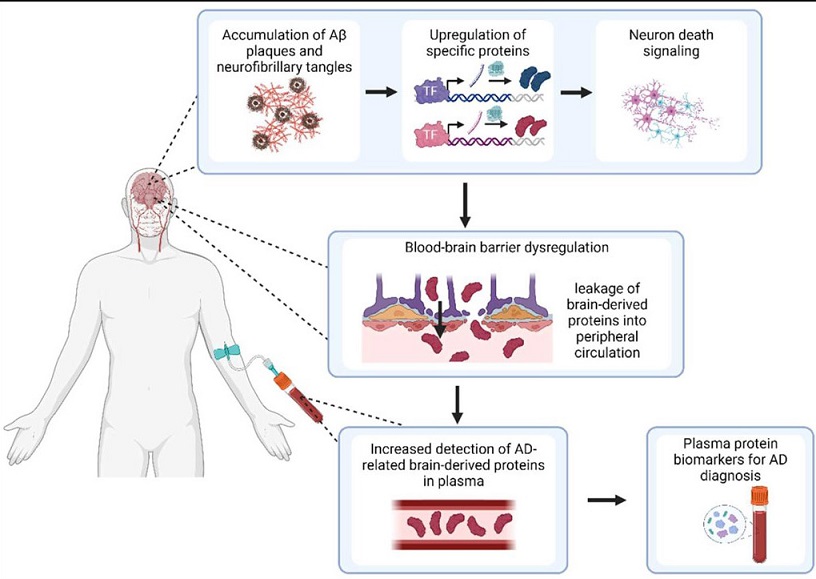
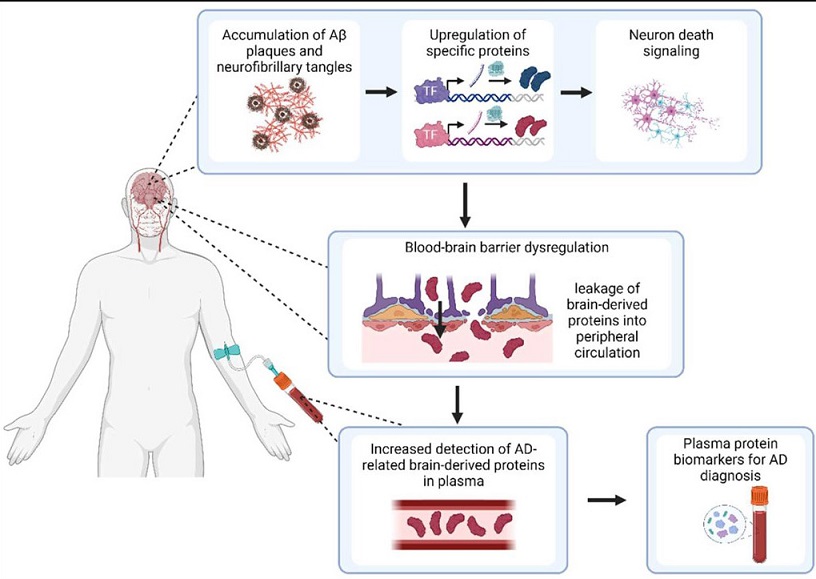 Scientists from Singapore Discover Plasma Biomarkers That Identify Blood-Brain Barrier Dysregulation in Alzheimer’s Disease. Overview of study hypothesis for detection of BBMs for AD.
Scientists from Singapore Discover Plasma Biomarkers That Identify Blood-Brain Barrier Dysregulation in Alzheimer’s Disease. Overview of study hypothesis for detection of BBMs for AD.
The study, led by researchers from Nanyang Technological University and the Bioinformatics Institute at A*STAR, Singapore, focused on finding specific proteins that leak from the brain into the bloodstream due to the breakdown of the blood-brain barrier. These proteins could serve as vital biomarkers for diagnosing Alzheimer’s disease, offering a non-invasive method for identifying the condition.
The Need for Better Diagnostics in Alzheimer’s
Alzheimer’s disease is one of the most common neurodegenerative disorders, characterized by memory loss, cognitive decline, and eventually, an inability to carry out everyday tasks. For years, doctors have relied on brain imaging techniques and cerebrospinal fluid tests to diagnose the condition. However, these methods are costly, invasive, and not always accessible to everyone.
Researchers have been searching for blood-based biomarkers as an easier and more affordable way to diagnose Alzheimer’s. Blood tests could help identify early signs of the disease, allowing for better treatment options and more time for patients and families to prepare for its progression. The Singaporean team’s findings could mark a significant step in that direction.
Understanding the Blood-Brain Barrier and Its Role in Alzheimer’s
The blood-brain barrier is a critical part of the body’s defense system. It protects the brain by preventing harmful substances from entering while allowing essential nutrients to pass through. In Alzheimer’s disease, however, this barrier begins to break down, leading to the leakage of certain proteins from the brain into the bloodstream.
This breakdown is thought to contribute to the progression of Alzheimer’s by allowing toxic substances to enter the brain and cause further damage to neurons. By identifying biomarkers that indicate blood-brain barrier dysregulation, scientists can detect this breakdown early and potentially intervene before the disease worsens.
Key Findings of the Study
The researchers identified five proteins - apolipoprotein D (APOD), beta-2 microglobulin (B2M), complement factor H (CFH), clusterin (CLU), and complement C3 (C3) - that serve as biomarkers for Alz
heimer’s disease. These proteins were found to be elevated in both the brain and the blood of patients with Alzheimer’s. Their presence in the blood suggests that they had leaked through the blood-brain barrier, providing a direct link between BBB dysfunction and Alzheimer’s.
-Apolipoprotein D (APOD): This protein is involved in lipid transport and has been linked to several neurodegenerative diseases, including Alzheimer’s. The researchers found that APOD levels were significantly higher in patients with Alzheimer’s compared to healthy individuals.
-Beta-2 Microglobulin (B2M): B2M is part of the immune system and plays a role in regulating immune responses. Its elevated levels in Alzheimer’s patients suggest it may be involved in the inflammatory processes associated with the disease.
-Complement Factor H (CFH): CFH is a protein that regulates the immune system’s complement pathway, which helps clear pathogens and damaged cells from the body. The researchers found that higher levels of CFH were associated with Alzheimer’s, indicating its role in the brain’s immune response to the disease.
-Clusterin (CLU): Clusterin is another protein involved in lipid transport and immune regulation. It has been found in amyloid plaques, one of the hallmark features of Alzheimer’s disease. The researchers noted that CLU levels were particularly elevated in patients with more advanced stages of the disease.
-Complement C3 (C3): Like CFH, C3 is part of the complement system and plays a crucial role in the body’s immune defense. Elevated levels of C3 in Alzheimer’s patients point to an overactive immune response in the brain, contributing to the disease’s progression.
How These Findings Could Change Alzheimer’s Diagnosis
One of the most promising aspects of this study is the potential for these biomarkers to be used in a simple blood test. Current methods of diagnosing Alzheimer’s, such as brain scans and spinal taps, are expensive and invasive. A blood test that measures levels of these five proteins could provide an easier, less costly way to diagnose the disease, particularly in its early stages.
This would be especially beneficial for patients in the early stages of Alzheimer’s when symptoms are mild or even unnoticeable. Early diagnosis allows for early intervention, which can slow the progression of the disease and improve the quality of life for patients and their families.
The Importance of Biological Validity
The researchers didn’t just stop at identifying these biomarkers; they also validated their findings by investigating the biological mechanisms behind the blood-brain barrier’s breakdown. They found that four of the biomarkers (APOD, B2M, CLU, and C3) were overexpressed in astrocytes, a type of brain cell that plays a crucial role in maintaining the blood-brain barrier.
Astrocytes are known to be affected by Alzheimer’s disease, and their dysfunction can contribute to the breakdown of the blood-brain barrier. By showing that these biomarkers are linked to changes in astrocytes, the researchers provided strong evidence that the proteins found in the blood are indeed coming from the brain.
Potential for Future Research
The discovery of these biomarkers opens up new avenues for research. Future studies could focus on understanding exactly how these proteins contribute to the progression of Alzheimer’s and whether they could be targeted for treatment.
Additionally, researchers could investigate whether these biomarkers are present in other neurodegenerative diseases, such as Parkinson’s disease or multiple sclerosis, to determine whether they are specific to Alzheimer’s or indicative of broader neurological issues.
Another area for future research could involve looking at whether these biomarkers can be used to predict the onset of Alzheimer’s before symptoms appear. If researchers can detect changes in these proteins years before cognitive decline begins, it could revolutionize the way we approach Alzheimer’s prevention and treatment.
Conclusion: A New Hope for Alzheimer’s Diagnosis
In conclusion, the discovery of these five plasma biomarkers offers new hope for diagnosing and understanding Alzheimer’s disease. The proteins identified in this study - APOD, B2M, CFH, CLU, and C3 - provide a direct link between blood-brain barrier dysfunction and Alzheimer’s disease. Their potential use in a blood test could lead to earlier and more accurate diagnoses, giving patients and doctors more time to intervene and manage the disease.
While more research is needed to fully understand the implications of these findings, this study represents a significant step forward in the fight against Alzheimer’s. By identifying biomarkers that are specific to the disease and linked to the breakdown of the blood-brain barrier, the researchers have opened the door to new diagnostic tools and potential treatments.
The study findings were published in the peer-reviewed journal: Frontiers in Bioinformatics.
https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2024.1463001/full
For the latest on Alzheimer’s Disease, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-news-study-reveals-potential-new-form-of-brain-neurodegeneration-linked-to-covid-19
https://www.thailandmedical.news/news/new-thailand-medical-study-reveals-link-between-oral-microbiota-and-alzheimer-s-disease