Singapore case study reveals that even mild COVID-19 can trigger fatal liver failure in patients with autoimmune liver disease
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 23, 2024 1 year, 2 months, 1 day, 8 hours, 14 minutes ago
Medical News: A recent case study has shocked the medical world as mild COVID-19 infection was found to trigger a fatal case of acute-on-chronic liver failure (ACLF) in a patient with autoimmune liver disease. Researchers from Duke-NUS Medical School-Singapore, A*STAR's Institute of Molecular and Cell Biology (IMCB)-Singapore, and Singapore General Hospital have detailed how a patient with a stable primary biliary cholangitis-autoimmune hepatitis (PBC-AIH) overlap syndrome experienced a rapid decline after contracting a mild form of COVID-19. This
Medical News report sheds light on how even a mild respiratory infection can cause severe complications in patients with preexisting liver conditions.
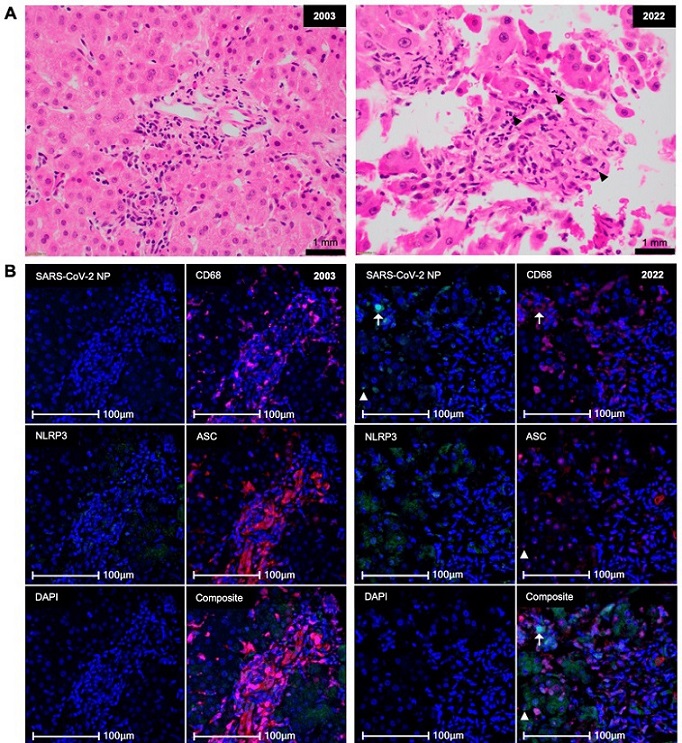
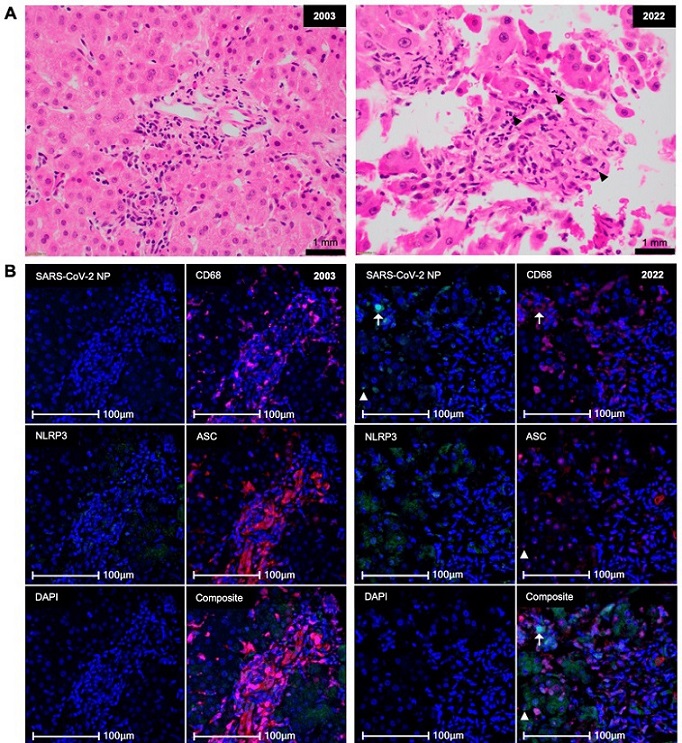 Limited SARS-CoV-2 infection but significant widespread inflammasome activation in the postmortem liver biopsy of the patient. (A,B) H&E and mIHC of liver biopsy at diagnosis (2003, left) and at time of death (2022, right). Black arrowheads, neutrophils. Cyan, SARS-CoV-2 NP; pink, CD68; green, NLRP3; red, ASC; blue, DAPI; arrows, SARS-CoV-2-infected NP+ CD68+ cells; arrowheads, NP+ ASC speck+ cells. Scale bars, 1 mm (A) and 100 µm (B).
Limited SARS-CoV-2 infection but significant widespread inflammasome activation in the postmortem liver biopsy of the patient. (A,B) H&E and mIHC of liver biopsy at diagnosis (2003, left) and at time of death (2022, right). Black arrowheads, neutrophils. Cyan, SARS-CoV-2 NP; pink, CD68; green, NLRP3; red, ASC; blue, DAPI; arrows, SARS-CoV-2-infected NP+ CD68+ cells; arrowheads, NP+ ASC speck+ cells. Scale bars, 1 mm (A) and 100 µm (B).
The case study outlines how the patient’s liver failure was driven by an inflammatory response known as inflammasome activation, which ultimately led to a fatal outcome. The findings provide new insights into how the immune system's overreaction to viral infections can have devastating consequences in vulnerable individuals. The study results emphasize the need for heightened vigilance in treating patients with chronic liver diseases, especially during the ongoing pandemic.
Case Report: A Devastating Decline
The subject of the study was a 58-year-old woman who had lived with PBC-AIH for nearly two decades. Her liver disease had been managed successfully, and while her condition was stable, she had been diagnosed with cirrhosis in the years leading up to her COVID-19 infection. Despite her chronic liver condition, the patient managed her symptoms well with medications, including ursodeoxycholic acid and azathioprine.
In March 2022, the patient contracted COVID-19. Notably, her symptoms were mild, and she was able to recover without any significant intervention. However, just weeks later, she began experiencing abdominal swelling due to ascites - an accumulation of fluid in the abdomen - a complication linked to her liver disease.
Over the next few months, her condition rapidly worsened. She required multiple hospitalizations and interventions, including large-volume paracentesis to drain the fluid. Despite intensive care, she developed complications such as spontaneous bacterial peritonitis, variceal hemorrhage, and hepatorenal syndrome, which eventually led to her death.
The question that baffled the medical team was how a mild COVID-19 infection could trigger such a rapid and catastrophic deterioration in a patient who had been relatively stable for years.
What the St
udy Found
The researchers discovered that the patient’s liver biopsy showed clear signs of inflammasome activation - a part of the body’s immune response that triggers inflammation. The inflammasome is a protein complex that responds to danger signals, such as infections, by producing proinflammatory cytokines like IL-1β and IL-18. These cytokines help the body fight infections but can also cause tissue damage if not regulated properly.
In this case, the inflammasome activation was likely triggered by the mild COVID-19 infection. The patient’s liver cells showed elevated levels of ASC specks, a hallmark of inflammasome activation. This suggests that the viral infection, while mild in the lungs, triggered a massive inflammatory response in her liver, which led to acute liver failure.
What was particularly striking about this case was that the level of liver cell death (hepatocyte pyroptosis) was minimal. This means that the patient’s liver cells were inflamed, but not dying in large numbers, which explains why her liver function appeared relatively preserved until the very end. However, the increased inflammation led to other complications, such as portal hypertension, which exacerbated her symptoms and led to her rapid decline.
Inflammasomes: The Silent Killer
The inflammasome is a double-edged sword. While it plays an important role in defending the body against infections, its overactivation can lead to harmful consequences, especially in individuals with preexisting conditions. In this case, the inflammasome activation in the liver was likely a result of the patient’s autoimmune liver disease being primed for such a response. COVID-19 served as the second hit, triggering the fatal inflammatory cascade.
Liver biopsies taken after the patient’s death showed significant inflammasome activation, particularly in the liver’s macrophages and hepatocytes. The study revealed that these liver cells were infected with SARS-CoV-2, though only at low levels, suggesting that even a mild or resolved COVID-19 infection could have long-lasting effects on the liver. The researchers also found elevated levels of proinflammatory cytokines like IL-18 and macrophage inhibition factor (MIF) in the patient’s blood, further confirming the presence of systemic inflammation.
The most puzzling aspect of the case was the patient’s lone hyperbilirubinemia - a condition where there is too much bilirubin in the blood - without a corresponding rise in other liver enzymes. This indicates that the bile ducts were likely affected by the inflammation, causing a build-up of bile that led to jaundice and further liver complications.
A New Understanding of COVID-19's Impact on Liver Disease
This study provides valuable insights into how even mild viral infections like COVID-19 can have severe consequences for patients with chronic liver diseases. While it has been well-documented that severe COVID-19 can cause liver damage, this case shows that even mild, self-limiting infections can trigger fatal outcomes in vulnerable populations. The researchers believe that the patient’s long-term use of immunosuppressant drugs, combined with her chronic liver disease, made her particularly susceptible to the inflammatory response that ultimately led to her death.
The study also raises important questions about how we should manage patients with chronic liver conditions during viral pandemics. Vaccination is crucial, but as this case shows, even fully vaccinated patients can experience severe complications. Monitoring patients for signs of inflammasome activation may be a key step in preventing similar outcomes in the future.
Conclusion
The findings of this study highlight the complex and often unpredictable nature of COVID-19 and its impact on the human body, particularly in patients with preexisting conditions. In this case, a mild infection triggered a fatal cascade of events, illustrating how dangerous the disease can be for those with chronic liver diseases. The research underscores the need for greater awareness of how viral infections can affect individuals with underlying conditions and the importance of early intervention.
Further research is needed to understand the exact mechanisms behind inflammasome activation and how it can be prevented. Developing new treatments that target inflammasomes, as well as better diagnostics to detect early signs of inflammation, could be critical in preventing similar outcomes in the future.
The study findings were published in the peer-reviewed journal: Viruses.
https://www.mdpi.com/1999-4915/16/10/1646
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/study-reveals-that-covid-19-is-causing-the-new-onset-of-acute-and-chronic-liver-disease-in-many
https://www.thailandmedical.news/news/new-study-findings-reveal-long-term-risks-of-liver-issues-from-covid-19