Small Extracellular Vesicles from Cord Blood Plasma and Placental Stem Cells Offer Hope for Treating Lung Injuries
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 26, 2024 4 months, 2 weeks, 2 hours, 11 minutes ago
Medical News: Lung injuries and complications arising from conditions such as sepsis and inflammation are major concerns for both newborns and adults. These complications can lead to chronic diseases like bronchopulmonary dysplasia (BPD), a condition primarily affecting premature infants who require long-term oxygen support. However, groundbreaking research by scientists from Michigan State University and Sparrow Hospital has unveiled a novel approach that could revolutionize treatment options.
 Small Extracellular Vesicles from Cord Blood Plasma and Placental Stem Cells Offer
Small Extracellular Vesicles from Cord Blood Plasma and Placental Stem Cells Offer
Hope for Treating Lung Injuries
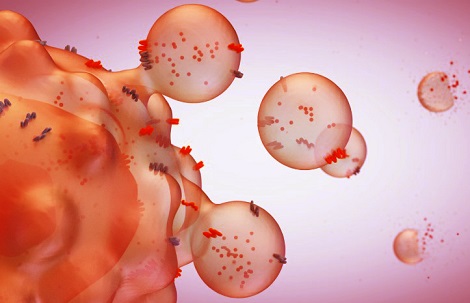
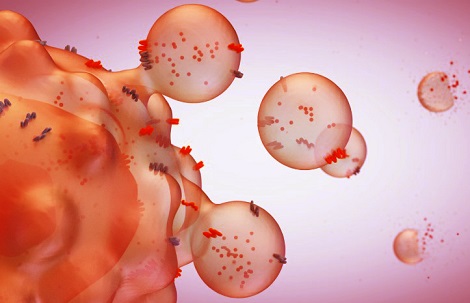
By using small extracellular vesicles (sEVs) derived from cord blood plasma (CBP) and placental mesenchymal stem cells (MSCs), researchers demonstrated the potential to combat lung injuries effectively. These vesicles, tiny particles secreted by cells, are filled with proteins, RNA, and other molecules that can influence immune responses and aid tissue repair.
Understanding the Study and Its Methods
This
Medical News report will guide readers through the recent findings, highlighting the mechanisms of action and potential clinical benefits of these sEVs. To investigate their effects, researchers collected sEVs from three sources: cord blood plasma, Wharton jelly (a part of the umbilical cord), and placental MSCs. These vesicles were isolated using advanced filtration and imaging techniques to ensure purity and efficacy.
Lung epithelial cells (A549) and immune cells (THP-1 monocytes) were exposed to a harmful substance called lipopolysaccharide (LPS), which is known to mimic severe bacterial infections. This allowed the team to simulate conditions seen in acute lung injury. The cells were then treated with the sEVs to observe their protective effects.
Key Findings from the Research
-Improved Cell Survival
LPS exposure led to significant cell damage and reduced survival rates in both lung and immune cells. However, when treated with sEVs from CBP, Wharton jelly, or placental MSCs, cell viability improved markedly. CBP-derived sEVs showed the strongest impact, suggesting a particularly potent therapeutic potential.
-Reduction in Inflammation
LPS triggers an intense inflammatory response, characterized by increased levels of cytokines such as interleukin-6 (IL-6) and interleukin-8 (IL-8). The study revealed that sEVs reduced these inflammatory markers. Interestingly, while Wharton jelly-derived sEVs suppressed both IL-6 and IL-8, CBP-derived sEVs displayed a mixed effect, reducing IL-6 but increasing IL-8 in certain cells.
-Prevention of Cell Death
One of the major benefits of sEV treatment was its ability to prevent apoptosis, or programmed cell death. By interfering with the mechanisms that drive cell damage, these vesicles helped maintain healthier cell populations, essential for tissue repair and recovery.
r />
Tailored Effects Based on Source
The researchers highlighted that the therapeutic benefits of sEVs are influenced by their source. This variability underscores the importance of selecting the appropriate type of vesicle for specific clinical applications.
Broader Implications of the Findings
The findings have profound implications for treating acute and chronic lung conditions. By modulating inflammation and promoting tissue repair, sEVs could potentially prevent the progression of diseases like BPD. Furthermore, their ability to target specific pathways in immune cells suggests they could also play a role in managing other inflammatory conditions.
Challenges and Future Directions
Despite the promising results, challenges remain. One limitation of this study was its focus on cell cultures. Future research will need to validate these findings in animal models and eventually in clinical trials. Additionally, the variability in sEV efficacy based on their source must be addressed. Standardizing production methods and characterizing the specific contents of these vesicles will be crucial steps toward their therapeutic use.
Another area for exploration is understanding how sEVs influence anti-inflammatory pathways. While this study primarily measured pro-inflammatory markers, the role of anti-inflammatory cytokines, such as IL-10, remains unclear.
Conclusions from the Research
In conclusion, this groundbreaking study highlights the immense potential of small extracellular vesicles derived from cord blood plasma and placental mesenchymal stem cells. These vesicles not only improve cell survival but also reduce inflammation and prevent cell death. As a result, they could offer a new lease on life for patients suffering from severe lung injuries and related conditions. However, further research is essential to address existing challenges and unlock the full therapeutic potential of these vesicles.
The study findings were published in the peer-reviewed International Journal of Molecular Sciences.
https://www.mdpi.com/1422-0067/26/1/75
For the latest in Medical Research, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/russian-scientist-turn-to-grapefruit-vesicles-to-transform-colon-cancer-treatment
https://www.thailandmedical.news/news/non-ionic-surfactant-vesicles-provide-new-hope-for-inflammation-treatment
https://www.thailandmedical.news/news/covid-19-study-links-extracellular-vesicles-to-severe-outcomes