Spanish Study Discovers That SARS-CoV-2 Infections Leads To Downregulation Of p53, A Critical Cancer Protective Gene!
Source: Medical News -SARS-CoV-2-An Oncogenic Virus Sep 12, 2022 3 years, 4 months, 1 week, 5 days, 16 hours, 54 minutes ago
Alarmingly more and more studies are emerging that are indicating SARS-CoV-2 infections will ultimately lead to the development of various cancers through a variety of mechanisms.
Thailand
Medical News had already covered an article that also includes links to existing studies that shows the various discovered mechanisms.
https://www.thailandmedical.news/news/breaking-study-finds-that-cancer-causing-genes-are-upregulated-in-sars-cov-2-infected-individuals
Spanish researchers from Universidade de Santiago de Compostela, Instituto de Salud Carlos III and the Hospital Clínico Universitario de Santiago (SERGAS) are also proposing that SARS-CoV-2 are also oncogenic viruses as they have found yet another mechanism by which SARS-CoV-2 infections can also contribute to the rise of cancers.
Based on previous works by German researchers in 2016 from the University of Lübeck and German Center for Infection Research, the Ludwig-Maximilians-University Munich, the Max-Planck Institute of Biochemistry and the University of Bonn Medical Centre that shows that the SARS-CoV virus along with other coronaviruses such as MERS-CoV, and HCoV-NL6 causes the downregulation of a critical cancer protective gene and protein called P53, the Spanish researchers also conducted studies that showed that SARS-CoV-2 also does the same if not even more.
https://www.pnas.org/doi/10.1073/pnas.1603435113
By stopping cells with mutated or damaged DNA from dividing, p53 helps prevent the development of cancers and tumors. Because p53 is essential for regulating DNA repair and cell division, it has been nicknamed the "guardian of the genome.
As p53 deficiency is so common in human cancer, the Spanish study findings that SARS-CoV-2 infections downregulates p53 has implications in the rise of cancers especially in Post COVID-19 individuals.
The Spanish researchers sent their study findings in the form of a correspondence to the peer reviewed Journal of Infection.
https://www.journalofinfection.com/article/S0163-4453(22)00469-8/fulltext
The study findings explain why COVID-19 could be a risk factor for developing cancer.
Typically, individuals infected with SARS-CoV-2 have a low presence of p53, a protein that is tumor-suppressive.
The study carried out by the University of Santiago de Compostela (USC) and the Health Research Institute (IDIS) in collaboration with Imperial College London, has focused on seeing how a tumor suppressor protein p53 responds to SARS-CoV-2.
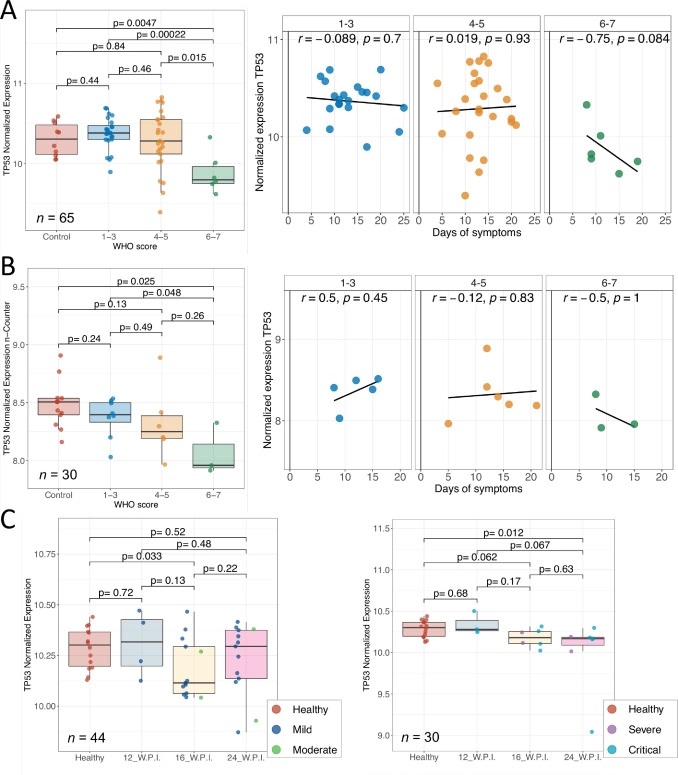
In the research, studies were carried out with healthy and SARS-CoV-2 infected patients stratified according to their severity, from critically ill, to severe, mild and healthy individuals. They were followed up at 12, 16 and 24 weeks, after having overcome the coronavirus infection.
The study findings showed that the SARS-CoV-2 antigens 'hij
ack' the onco-suppressor protein p53, leading to its degeneration due to oxidative damage.
The findings indicted that the SARS-CoV-2 virus would take advantage of the pathways controlled by p53 during the infection phase, bypassing immune responses.
The study findings also showed that patients in the acute phase of SARS-CoV-2 and those with long-term infection (known as persistent COVID) showed a low presence of p53.
The study team warns that the long-term inhibition of p53 by SARS-CoV-2 could be a carcinogenic risk factor.
The study team said, "This does not demonstrate a causal relationship between SARS-CoV-2 and cancer, we are confident that a larger sample study and extensive follow-up studies can confirm what we are proposing and the impact of this finding on global public health would be enormous.”
Already, two earlier Chinese studies also published in the same journal ie Journal of Infection, had found that SARS-CoV-2 contributed to severe endometrial cancer in many women.
https://pubmed.ncbi.nlm.nih.gov/35561867/
https://pubmed.ncbi.nlm.nih.gov/35077768/
The Spanish study team said, “Our study findings originates from the realm of gene expression, what we call transcriptomics. The fact that we found converging evidence in independent studies lays a solid enough base to start studies in the clinical and epidemiological field that allow shedding light on this possible link.”
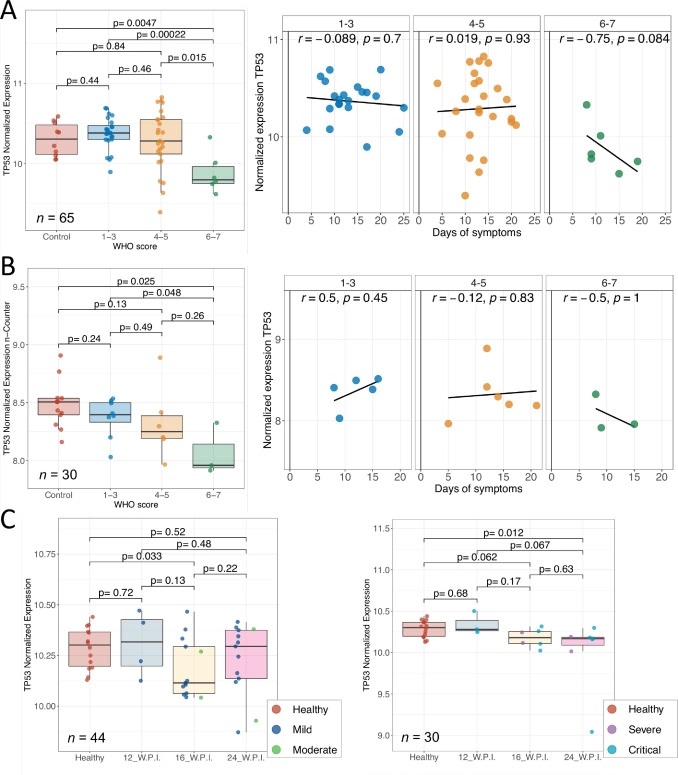 (A) TP53 gene expression in blood samples from COVID-19 patients and healthy controls from the RNAseq dataset and stratified by WHO severity score (left). Correlation between days of symptoms to sample collection and TP53 expression in the RNAseq dataset (right). (B) TP53 gene expression in blood samples from COVID-19 patients and healthy controls from the n-Counter dataset and stratified by WHO severity score (left); patients from this cohort partially overlap with those in the RNAseq dataset. Correlation between days of symptoms to sample collection and TP53 expression in the n-Counter dataset (right). Asymptomatic patients were not included in the correlation analyses (r = spearman correlation coefficient). (C) TP53 gene expression in blood samples from mild/moderate (left) and severe/critical (right) long-COVID-19 patients as well as healthy controls collected at different timepoints post infection (w.p.i = weeks post infection).
(A) TP53 gene expression in blood samples from COVID-19 patients and healthy controls from the RNAseq dataset and stratified by WHO severity score (left). Correlation between days of symptoms to sample collection and TP53 expression in the RNAseq dataset (right). (B) TP53 gene expression in blood samples from COVID-19 patients and healthy controls from the n-Counter dataset and stratified by WHO severity score (left); patients from this cohort partially overlap with those in the RNAseq dataset. Correlation between days of symptoms to sample collection and TP53 expression in the n-Counter dataset (right). Asymptomatic patients were not included in the correlation analyses (r = spearman correlation coefficient). (C) TP53 gene expression in blood samples from mild/moderate (left) and severe/critical (right) long-COVID-19 patients as well as healthy controls collected at different timepoints post infection (w.p.i = weeks post infection).
The Spanish study team concluded, “SARS-CoV-2 is now a contributing risk factor various types of cancer besides genetic mutations and environmental factors.”
It should be noted that in the 2016 German study, the researchers identified cellular E3 ubiquitin ligase ring-finger and CHY zinc-finger domain-containing 1 (RCHY1) as an interacting partner of the viral SARS-CoV unique domain (SUD) and papain-like protease (PLpro), and, as a consequence, the involvement of cellular p53 as antagonist of coronaviral replication.
Residues 95–144 of RCHY1 and 389–652 of SUD (SUD-NM) subdomains are crucial for interaction. Association with SUD increases the stability of RCHY1 and augments RCHY1-mediated ubiquitination as well as degradation of p53.
Interestingly, the calcium/calmodulin-dependent protein kinase II delta (CAMK2D), which normally influences RCHY1 stability by phosphorylation, also binds to SUD. In vivo phosphorylation shows that SUD does not regulate phosphorylation of RCHY1 via CAMK2D.
In the same light as the SUD, the PLpros from SARS-CoV, MERS-CoV, and HCoV-NL63 physically interact with and stabilize RCHY1, and thus trigger degradation of endogenous p53.
The SARS-CoV papain-like protease is encoded next to SUD within nonstructural protein 3. A SUD–PLpro fusion interacts with RCHY1 more intensively and causes stronger p53 degradation than SARS-CoV PLpro alone.
The study findings demonstrated that p53 inhibits replication of infectious SARS-CoV as well as of replicons and human coronavirus NL63.
Hence, human coronaviruses antagonize the viral inhibitor p53 via stabilizing RCHY1 and promoting RCHY1-mediated p53 degradation. SUD functions as an enhancer to strengthen interaction between RCHY1 and nonstructural protein 3, leading to a further increase in in p53 degradation.
The significance of these findings is that down-regulation of p53 as a major player in antiviral innate immunity provides a long-sought explanation for delayed activities of respective genes.
The German study team concluded, “Severe acute respiratory syndrome coronavirus (SARS-CoV) is one of the most pathogenic human coronaviruses. Virulence is reflected in the molecular interplay between virus and host cells. Here we show a strategy of how SARS-CoV antagonizes the host antiviral factor p53, which impairs viral replication. The papain-like protease of the nonstructural protein 3 of SARS-CoV and other coronaviruses physically interact with and stabilize E3 ubiquitin ligase ring-finger and CHY zinc-finger domain-containing 1 (RCHY1), thereby augmenting RCHY1-mediated degradation of p53. The SARS-unique domain (SUD) enhances these effects. Knockout of p53 promotes replication of SARS-CoV replicons and of infectious virus. Taken together we identify cellular p53 as antiviral measure of coronavirus-infected cells, which is counteracted via the stabilization of RCHY1 by viral SUD and papain-like protease (PLpro) proteins and via ubiquitination of p53.”
As SARS-CoV-2 is even more ‘enhanced’ than SARS-CoV, it is also suspected that the downregulation of p35 by SARS-CoV-2 is of a greater fold than that of SARS-CoV.
For the latest on
SARS-CoV-2 and Cancers, keep on logging to Thailand
Medical News.