Staff Writer, TMN Jul 04, 2018 7 years, 6 months, 2 weeks, 6 days, 1 hour, 59 minutes ago
Cancer is the leading cause of death across the globe. For years now, researchers have led meticulous studies focused on how to stop this deadly disease in its tracks. How close are we to finding more effective treatments?
The World Health Organization (WHO) note that, worldwide, nearly
1 in 6 deaths are down to
cancer.
In the United States alone, the National Cancer Institute (NCI)
estimated 1,688,780 new cancer cases and 600,920 cancer-related deaths in 2017.
Currently, the most common types of are
chemotherapy,
radiotherapy,
tumor surgery, and — in the case
prostate cancer and
breast cancer — hormonal therapy.
However, other types of treatment are beginning to pick up steam: therapies that — on their own or in combination with other treatments — are meant to help defeat cancer more efficiently and, ideally, have fewer side effects.
Innovations in cancer treatment aim to address a set of issues that will typically face
healthcare providers and patients, including aggressive treatment accompanied by unwanted side effects, tumor recurrence after treatment, surgery, or both, and aggressive cancers that are resilient to widely utilized treatments.
Below, we review some of the most recent cancer research breakthroughs that give us renewed hope that better therapies and prevention strategies will soon follow suit.
Boosting the immune system's 'arsenal'
One type of therapy that has attracted a lot of attention recently is
immunotherapy, which aims to reinforce our own bodies' existing arsenal against foreign bodies and harmful cells: our immune system's response to the spread of cancer tumors.
But many types of cancer cell are so dangerous because they have ways of "duping" the immune system — either into
ignoring them altogether or else into giving them a "
;helping hand."
Therefore, some types of aggressive cancer are able to spread more easily and become resistant to chemotherapy or radiotherapy.
However, thanks to in vitro and in vivo experiments, researchers are now learning how they might be able to "deactivate" the cancer cells' protective systems. A
study published last year in
Nature Immunology found that macrophages, or white blood cells, that are normally tasked with "eating up" cellular debris and other harmful foreign "objects" failed to obliterate the super-aggressive cancer cells.
That was because, in their interaction with the cancer cells, the macrophages read not one but two signals meant to repel their "cleansing" action.
This knowledge, however, also showed the scientists the way forward: by blocking the two relevant signaling pathways, they re-enabled the white blood cells to do their work.
Therapeutic viruses and innovative 'vaccines'
A surprising weapon in the fight against cancer could be
therapeutic viruses, as revealed by a team from the United Kingdom earlier this year. In their experiments, they managed to use a
reovirus to attack brain cancer cells while leaving healthy cells alone.
"This is the first time it has been shown that a therapeutic virus is able to pass through the brain-blood barrier," explained the study authors, which "opens up the possibility [that] this type of immunotherapy could be used to treat more people with aggressive brain cancers."
Another area for improvement in immunotherapy is "dendritic vaccines," a strategy wherein dendritic cells (which play a key role in the body's immune response) are collected from a person's body, "armed" with tumor-specific antigens — which will teach them to "hunt" and destroy relevant cancer cells — and injected back into the body to boost the immune system.
In a
new study, researchers in Switzerland identified a way to improve the action of these dendritic vaccines by creating artificial receptors able to recognize and "abduct" tiny vesicles that have been linked to cancer tumors' spread in the body.
By attaching these artificial receptors to the dendritic cells in the "vaccines," the therapeutic cells are enabled to recognize harmful cancer cells with more accuracy.
Importantly, recent studies have shown that immunotherapy may work best if delivered
in tandem
with chemotherapy — specifically, if the chemotherapy drugs are delivered first, and they are followed up with immunotherapy.
But this approach does have some pitfalls; it is difficult to control the effects of this combined method, so sometimes, healthy tissue may be attacked alongside cancer tumors.
However, scientists from two institutions in North Carolina have developed a substance that, once injected into the body, becomes gel-like: a "
bioresponsive scaffold system." The scaffold can hold both chemotherapy and immunotherapy drugs at once, releasing them systematically into primary tumors.
This method allows for a better control of both therapies, ensuring that the drugs act on the targeted tumor alone.
The nanoparticle revolution
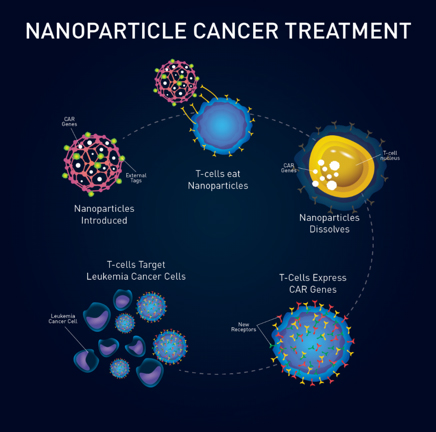
Speaking of specially developed tools for delivering drugs straight to the tumor and hunting down micro tumors with accuracy and efficiency, the past couple of years have seen a "boom" in nanotechnology and nanoparticle developments for cancer treatments.
Nanoparticles are microscopic particles that have garnered so much attention in clinical research, among other fields, because they bring us the chance to develop precise, less invasive methods of tackling disease.
Example of how nanoparticles work in as a cancer cure
Vitally, they can target cancer cells or cancer tumors without harming healthy cells in the surrounding environment.
Some nanoparticles have now been created to provide very focused hyperthermic treatment, which is a type of therapy that uses hot temperatures to make cancer tumors shrink.
Last year, scientists from China and the U.K. managed to come up with a type of "
self-regulating" nanoparticle that was able to expose tumors to heat while avoiding contact with healthy tissue.
"This could potentially be a game-changer in the way we treat people who have cancer," said one of the researchers in charge of this project.
These tiny vehicles can also be used to target
cancer stem-like cells, which are undifferentiated cells that have been linked to the resilience of certain types of cancer in the face of traditional treatments such as chemotherapy.
Thus, nanoparticles can be "loaded" with drugs and set to "hunt down" cancer
stem cells to
prevent the growth or recurrence of tumors. Scientists have experimented with drug-filled nanoparticles in the treatment of various types of cancer, including breast cancer and
endometrial cancer.
No less importantly, minuscule vehicles called "
nanoprobes" can be used to detect the presence of micrometastases, which are secondary tumors so tiny that they cannot be seen using traditional methods.
Dr. Steven K. Libutti, director of the Rutgers Cancer Institute of New Jersey in New Brunswick, calls micrometastases "the Achilles' heel of surgical management for cancer" and argues that nanoprobes "go a long way to solving [such] problems."
Tumor 'starvation' strategies
Another type of strategy that researchers have been investigating of late is that of "starving" tumors of the nutrients they need to grow and spread. This, scientists point out, could be a saving grace in the case of aggressive, resilient cancers that cannot effectively be eradicated otherwise.
Three different studies — whose results were all published in January this year — looked at ways of cutting off cancers' nutritional supplies.
One of these studies looked at ways of
stopping glutamine, a naturally occurring amino acid, from feeding cancer cells.
Certain cancers, such as breast, lung, and colon, are known to use this amino acid to support their growth.
By blocking cancer cells' access to glutamine, the researchers managed to maximize the impact of oxidative stress, a process that eventually induces cell death, on these cells.
Some aggressive types of breast cancer may be halted by stopping the cells from "feeding" on a particular enzyme that helps them to
produce the energy they need to thrive.
Another way of depleting cancer cells of energy is by blocking their
access to vitamin B-2, as researchers from the University of Salford in the U.K. have observed.
As one study author says, "This is hopefully the beginning of an alternative approach to halting cancer stem cells." This strategy could help individuals receiving cancer treatment to avoid the toxic side effects of chemotherapy.
Cancer treatments and epigenetics
Epigenetics refers to the changes caused in our bodies by alterations in gene expression, which dictate whether certain characteristics appear or if certain "actions" are affected at a biological level.
According to research that addressed the impact of such changes, many cancers, as well as the behaviors of cancer cells, are determined by
epigenetic factors.
"Recent advances in the field of epigenetics have shown that human cancer cells harbor global epigenetic abnormalities, in addition to numerous genetic alterations."
"These genetic and epigenetic alterations interact at all stages of cancer development, working together to promote cancer progression."
Thus, it is crucial for specialists to understand when and where to intervene and the expression of which genes they may need to switch on or off, depending on their role in the development of cancer.
One
study, for instance, found that the gene responsible for the advent of
Huntington's diseaseproduces a set of molecules whose action may actually prevent cancer from occurring.
Now, the researchers' challenge is to channel the therapeutic potential of this process without triggering Huntington's disease. However, the scientists are hopeful.
"We believe a short-term treatment cancer therapy for a few weeks might be possible," says the study's senior author.
Another recent study was able to establish that estrogen-receptor positive breast cancers that become resistant to chemotherapy gain their resilience through
genetic mutations that "confer a metastatic advantage to the tumor.
"
But this knowledge also gave researchers the "break" that they needed to come up with an improved treatment for such stubborn tumors: a combination therapy that delivers the chemotherapeutic drug fulvestrant alongside an experimental enzyme inhibitor.
What does this all mean?
Cancer research is running at full speed, taking advantage of all the technological advances that science has achieved over recent years. But what does that mean in terms of coming up with a cure for cancer?
Whether or not there will ever be a cure for all cancer types is currently a matter of strong debate; although promising studies are published and covered by the media almost every day, cancer types vary immensely.
This makes it very difficult to say that an approach that works for one type will be adaptable to all.
Also, while there is much emerging research promising more effective treatments, most of these projects are still in their early stages, having conducted in vitro and in vivo experiments. Some potential treatments still have a long way to go before clinical trials in human patients
.
Still, that doesn't mean we should lose all hope. Some researchers
explain that these efforts should make us optimistic; while we may not be at the stage where we can claim that cancer can easily be eradicated, our furthered knowledge and ever more precise tools keep us ahead of the game and improve our odds in the fight against this disease.